The first experience of combined treatment of brain malignant gliomas by means of blocking membrane calcium channels
DOI:
https://doi.org/10.25305/unj.168800Keywords:
glioblastomas, tumor-associated inflammation, NMDA receptors, blood cell aggregation, surface plasmon resonance, biosensor, verpamil hydrochloride, low concentrationsAbstract
Objective. To investigate the antitumor effect of low concentrations of calcium channel blockers on the example of verapamil hydrochloride in the combined treatment of patients with glioblastomas after operation.
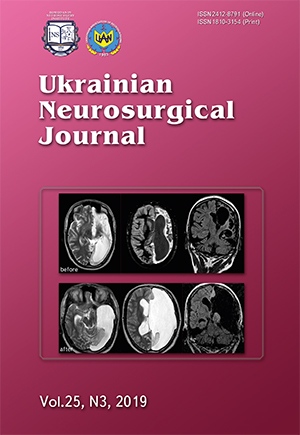
Materials and methods. Patients who underwent brain tumor surgery, postoperative radiotherapy and chemotherapy were divided into two groups. The first group of 8 patients received verapamil hydrochloride at low concentrations; the second group (32 patients) served as a control group. The drug concentration was selected individually according to peripheral blood cells aggregation data on the “Plasmon-6” biosensor. The criterion for selecting the drug concentration was the lowest level of peripheral blood cells aggregation in vitro, reflecting the level of blocking of NMDA-dependent calcium channels on the membranes of peripheral blood cells. The optimal concentration of verapamil hydrochloride for all patients was less than 10,000 times less compared to common dose. The criteria of the antitumor activity of verapamil hydrochloride at low concentrations was the postoperative life expectancy of the patients.
Results. When using the drug in patients, there were no signs of toxic effects of verapamil hydrochloride on the body, and life expectancy was 10 months more compared to the group of patients not treated with verapamil hydrochloride at low concentrations in the postoperative period.
Conclusions. There was an increase in the life expectancy and improvement of the quality of life in patients who received treatment with low concentrations of verapamil hydrochloride, along with the absence of the toxic and tumor-stimulating action of the drug.
References
1. Matsko DE. Neyrokhirurgicheskaya patologiya. Rukovodstvo. St. Petersburg: RNKHI im. prof. AL Polenova. 2012. Russian.
2. Zozulya YuA, Vasil’yeva IG, Glavatskiy AYa, Rozumenko VD, Lisyaniy NI, Gridina NY. Sovremenniye tekhnologii konservativnogo lecheniya gliom. In: Zozulya YuA, editor. Gliomy golovnogo mozga. Kiev: UIPK “EeksOb”; 2007. P.383-509. Russian.
3. Luchnik AN. [A common link in the mechanism of the self-maintenance of malignant growth: the syndrome of the nonhealing wound]. Ontogenez. 2000 May-Jun;31(3):227-31. Russian. [PubMed]
4. Schwarzburd PM. [Chronic inflammation increases risk of epithelial neoplasia by inducing precancerous microenvironment: an evaluation of pathways of disregulation]. Vopr Onkol. 2006;52(2):137-44. Russian. [PubMed]
5. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008 Jul; 454 (7203):436-44. [CrossRef] [PubMed]
6. Whiteside TL. The tumor microenvironment and its role in promoting tumor growth. Oncogene. 2008 Oct 6;27(45):5904-12. [CrossRef] [PubMed] [PubMed Central]
7. Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002 Jun;2(6):442-54. [CrossRef] [PubMed]
8. Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009 Apr;9(4):265-73. [CrossRef] [PubMed]
9. Gridina N, Maslov V, Ushenin Yu. Tumor-Associated Inflammation and Brain Glyomas. Saarbrücken, Lambert Academic Publishing; 2013. 196 p. Russian.
10. Takano T, Lin JH, Arcuino G, Gao Q, Yang J, Nedergaard M. Glutamate release promotes growth of malignant gliomas. Nat Med. 2001 Sep;7(9):1010-5. [CrossRef] [PubMed]
11. Fu YS, Lin YY, Chou SC, Tsai TH, Kao LS, Hsu SY, Cheng FC, Shih YH, Cheng H, Fu YY, Wang JY. Tetramethylpyrazine inhibits activities of glioma cells and glutamate neuro-excitotoxicity: potential therapeutic application for treatment of gliomas. Neuro Oncol. 2008 Apr; 10 (2): 139-52. [CrossRef] [PubMed] [PubMed Central]
12. Gridina NY. Utilizing SPR as a novel technique to measure cell aggregation for ketamine treated brain gliomas. Cancer and Oncology Research. 2013 Jul;1(1):1-5. [CrossRef]
13. Clements JD, Lester RA, Tong G, Jahr CE, Westbrook GL. The time course of glutamate in the synaptic cleft. Science. 1992 Nov 27;258(5087):1498-501. [CrossRef] [PubMed]
14. Davydova ON, Boldyrev AA. Glutamate recep tors in neuronal and immune system cells. Ann Klin Eksp Nevrol. 2007;(4):28-34. Russian.
15. Gridina NY, Shvachko LP, Draguntsova NG. Tumor-Associated Inflammation Mechanisms Correction by Verapamil at Brain Gliomas Progression. Eur J Pharmaceutic Med Res (EJPMR). 2016;3(8):73-78. Available from: https://www.ejpmr.com/admin/assets/article_issue/1469854979.pdf
16. Medyanik IA. New approaches to early diagnosis and treatment tactics for malignant brain tumors (clinical and experimental research) [dissertation]. Nizhny Novgorod: VA Almazov North-West Federal Medical Research Center; 2016. Russian.
17. Karpov IuA, Soboleva GN. [Calcium antagonists--the first-line preparations in modern cardiology (II)]. Ter Arkh. 1997;69(1):74-8. Russian. [PubMed]
18. Mokhort NA, Seredinskaya NN, Bobkova LS. Calcium antagonists: prospects for new medical preparations development (review of literature). Journal of AMS of Ukraine. 2003;9(1):15-27. Russian.
19. Soybir G, Köksoy F, Koyuncu H, Yalçin O, Köse H, Topuzlu C. Chemoprevention of DMBA-induced mammary gland carcinogenesis--preventive effects of free oxygen radical scavengers. Breast Cancer Res Treat. 1998 Jul;50(2):193-9. [CrossRef] [PubMed]
20. Dunn AJ, Faust J, Krowech G. Evidence on the carcinogenicity of verapamil. California: OEHHA; 2004. 45 p. Available from: https://oehha.ca.gov/media/downloads/proposition-65/chemicals/hidverapamil.pdf
21. Helson L. Calcium channel blocker enhancement of anticancer drug cytotoxicity - a review. Cancer Drug Deliv. 1984;1(4):353-61. [CrossRef] [PubMed]
22. Gridina NYa, Maslov VP, Kotovsky VY, Draguntsova NG. Peculiarities of the Spectrum of Chromosome Aberrations in the Peripheral Blood Lymphocytes in Cases of Brain Gliomas and their Correction with Verapamil and Ketamine. Scholar Journal of Applied Medical Sciences (SJAMS). 2015 Sep;3(6A):2156-2160. Available from: http://saspublisher.com/wp-content/uploads/2015/09/SJAMS-36A-2156-2160.pdf
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Nina Ya. Gridina, Filia I. Zhebrivska, Аnatoly M. Morozov, Volodymyr D. Rozumenko, Yuri V. Ushenin, Аrtem V. Rozumenko, Аnnа А. Shmeleva, Аnnа D. Bilousova, Vadym V. Biloshytsky

This work is licensed under a Creative Commons Attribution 4.0 International License.
Ukrainian Neurosurgical Journal abides by the CREATIVE COMMONS copyright rights and permissions for open access journals.
Authors, who are published in this Journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the Journal under the terms of Creative Commons Attribution License, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this Journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form of which it has been published by the Journal (for example, to upload the work to the online storage of the Journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this Journal is included.