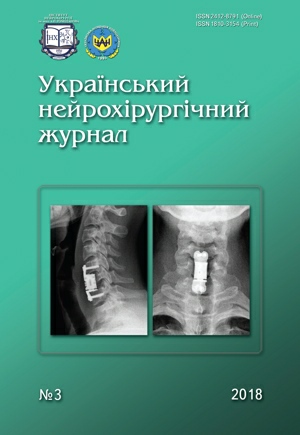
Dynamics of pain intensity in patients after anterior subaxial cervical fusion
DOI:
https://doi.org/10.25305/unj.139968Keywords:
pain, anterior cervical fusion, vertebral body replacement implant, numeral rating scaleAbstract
Objective: to study dynamics of pain intensity in patients undergone anterior subaxial cervical fusion depending on the type of fixing construction.
Materials and Methods. Thirty-five patients were operated for traumatic cervical spine injury: resection of the damaged vertebral body and fusion with vertical cylindrical implant types Mesh combined with ventral plate (29 patients) or telescopic vertebral body replacement implant (24 patients). The pain intensity was evaluated during observation period: before surgery, after 5–7 days, 3 months, 6 months and 12–18 months after operation using a numeral rating scale.
Results. The data obtained demonstrate the benefit of using telescopic vertebral body replacement implant that is evident as a lower level of pain intensity in patients in the postoperative period. The studied index difference is statistically significant in observation terms of 5–7 days and 3 months. The gradual leveling of differences between the groups is observed with 12–18 months after surgery.
Conclusion. The type of fusion system when used during surgery has a great influence on the pain duration in the postoperative period. Optimal selection of implant design can improve the quality of life in patients after anterior subaxial cervical fusion.
References
1. Lee SH, Lee JC, Tauchi R, Daniel Riew K. Influence of the Number of Cervical Fusion Levels on Cervical Spine Motion and Health-Related Quality of Life. Spine (Phila Pa 1976). 2016 Apr;41(8):E474-80. [CrossRef] [PubMed]
2. Hatch MN, Cushing TR, Carlson GD, Chang EY. Neuropathic pain and SCI: Identification and treatment strategies in the 21st century. J Neurol Sci. 2018 Jan 15;384:75-83. [CrossRef] [PubMed]
3. Arts MP, Peul WC. Vertebral body replacement systems with expandable cages in the treatment of various spinal pathologies: a prospectively followed case series of 60 patients. Neurosurgery. 2008 Sep;63(3):537-44; discussion 544-5. [CrossRef] [PubMed]
4. Elder BD, Lo SF, Kosztowski TA, Goodwin CR, Lina IA, Locke JE, Witham TF. A systematic review of the use of expandable cages in the cervical spine. Neurosurg Rev. 2016 Jan;39(1):1-11; discussion 11. [CrossRef] [PubMed]
5. Ames CP. Erratum: Expandable cylindrical cages in the cervical spine: a review of 22 cases. J Neurosurg Spine. 2016 Dec;25(6):795. [PubMed]
6. Koller H, Schmidt R, Mayer M, Hitzl W, Zenner J, Midderhoff S, Graf N, Resch H, Wilke HJ. The stabilizing potential of anterior, posterior and combined techniques for the reconstruction of a 2-level cervical corpectomy model: biomechanical study and first results of ATPS prototyping. Eur Spine J. 2010 Dec;19(12):2137-48. [CrossRef] [PubMed] [PubMed Central]
7. Fischer CR, Cassilly R, Cantor W, Edusei E, Hammouri Q, Errico T. A systematic review of comparative studies on bone graft alternatives for common spine fusion procedures. Eur Spine J. 2013 Jun;22(6):1423-35. [CrossRef] [PubMed] [PubMed Central]
8. Sewell MD, Rothera L, Stokes O, Clarke A, Hutton M. Assessing the amount of distraction needed for expandable anterior column cages in the cervical spine. Ann R Coll Surg Engl. 2017 Nov;99(8):659-660. [CrossRef] [PubMed] [PubMed Central]
9. Shen Y, Du W, Wang LF, Dong Z, Wang F. Comparison of Zero-profile Device Versus Plate-and-Cage Implant in the Treatment of Symptomatic Adjacent Segment Disease after Anterior Cervical Discectomy and Fusion: A Minimum 2-Year Follow-Up Study. World Neurosurg. 2018 Jul;115:e226-e232. [CrossRef] [PubMed]
10. Shaw KA, Griffith M, Mottern ET, Gloystein DM, Devine JG. Preventing Construct Subsidence Following Cervical Corpectomy: The Bump-stop Technique. Asian Spine J. 2018 Feb;12(1):156-161. [CrossRef] [PubMed] [PubMed Central]
11. Ordway NR, Rim BC, Tan R, Hickman R, Fayyazi AH. Anterior cervical interbody constructs: effect of a repetitive compressive force on the endplate. J Orthop Res. 2012 Apr;30(4):587-92. [CrossRef] [PubMed]
12. Weber MH, Fortin M, Shen J, Tay B, Hu SS, Berven S, Burch S, Chou D, Ames C, Deviren V. Graft Subsidence and Revision Rates Following Anterior Cervical Corpectomy: A Clinical Study Comparing Different Interbody Cages. Clin Spine Surg. 2017 Nov;30(9):E1239-E1245. [CrossRef] [PubMed]
13. Nekhlopochin AS, Nekhlopochin SN, Syrovoy GV. The analysis of stress-strain state in the cortical screw-vertebral body system when modelling of fixation of implants for anterior cervical interbody fusion. Russ J Biomech. 2017;21(1):77–88. [CrossRef]
14. Slynko II, Nekhlopochin AS. The clinically and biomechanically based optimization of sagittal contour surgical correction of the injured segment with the anterior subaxial fusion. MOJ App Bio Biomech. 2018;2(2):150–5. [CrossRef]
15. Brenke C, Fischer S, Carolus A, Schmieder K, Ening G. Complications associated with cervical vertebral body replacement with expandable titanium cages. J Clin Neurosci. 2016 Oct;32:35-40. [CrossRef] [PubMed]
16. Magu S, Singh D, Yadav RK, Bala M. Evaluation of Traumatic Spine by Magnetic Resonance Imaging and Correlation with Neurological Recovery. Asian Spine J. 2015 Oct;9(5):748-56. [CrossRef] [PubMed] [PubMed Central]
17. Wang T, Ma L, Yang DL, Wang H, Bai ZL, Zhang LJ, Ding WY. Factors predicting dysphagia after anterior cervical surgery: A multicenter retrospective study for 2 years of follow-up. Medicine (Baltimore). 2017 Aug;96(34):e7916. [CrossRef] [PubMed] [PubMed Central]
18. Passias PG, Poorman GW, Segreto FA, Jalai CM, Horn SR, Bortz CA, Vasquez-Montes D, Diebo BG, Vira S, Bono OJ, De La Garza-Ramos R, Moon JY, Wang C, Hirsch BP, Zhou PL, Gerling M, Koller H, Lafage V. Traumatic Fractures of the Cervical Spine: Analysis of Changes in Incidence, Cause, Concurrent Injuries, and Complications Among 488,262 Patients from 2005 to 2013. World Neurosurg. 2018 Feb;110:e427-e437. [CrossRef] [PubMed]
19. Feuchtbaum E, Buchowski J, Zebala L. Subaxial cervical spine trauma. Curr Rev Musculoskelet Med. 2016 Dec;9(4):496-504. [PubMed] [PubMed Central]
20. Shashua A, Geva Y, Levran I. Translation, Validation, and Crosscultural Adaptation of the Hebrew Version of the Neck Disability Index. Spine (Phila Pa 1976). 2016 Jun;41(12):1036-40. [CrossRef] [PubMed]
21. Schomberg D, Miranpuri G, Duellman T, Crowell A, Vemuganti R, Resnick D. Spinal cord injury induced neuropathic pain: Molecular targets and therapeutic approaches. Metab Brain Dis. 2015 Jun;30(3):645-58. [CrossRef] [PubMed]
22. Wu J, Luo D, Ye X, Luo X, Yan L, Qian H. Anatomy-related risk factors for the subsidence of titanium mesh cage in cervical reconstruction after one-level corpectomy. Int J Clin Exp Med. 2015 May 15;8(5):7405-11. eCollection 2015. [PubMed] [PubMed Central]
23. Barysh O, Buznytsky R. Anterior interbody cervicospondylodesis with use of vertical cylindrical mesh implants. Orthopaedics, traumatology and prosthetics. 2010;4:50–5. Russian. [CrossRef]
24. Nekhlopochin AS, Shvets AI, Nekhlopochin SN. [A telescopic vertebral endoprosthesis for subaxial cervical fusion]. Zh Vopr Neirokhir Im N N Burdenko. 2016;80(1):19-26. English, Russian. [CrossRef] [PubMed]
25. Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011 Oct;152(10):2399-404. [CrossRef] [PubMed]
26. Brunelli C, Zecca E, Martini C, Campa T, Fagnoni E, Bagnasco M, Lanata L, Caraceni A. Comparison of numerical and verbal rating scales to measure pain exacerbations in patients with chronic cancer pain. Health Qual Life Outcomes. 2010 Apr 22;8:42. [CrossRef] [PubMed] [PubMed Central]
27. Ughratdar I, Muquit S, Sivakumar G, White BD. A simple method to ease insertion and removal of vertebral body distractor pins in anterior cervical surgery. Br J Neurosurg. 2013 Feb;27(1):141-2. [CrossRef] [PubMed]
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2018 Ievgenii I. Slynko, Alexey S. Nekhlopochin

This work is licensed under a Creative Commons Attribution 4.0 International License.
Ukrainian Neurosurgical Journal abides by the CREATIVE COMMONS copyright rights and permissions for open access journals.
Authors, who are published in this Journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the Journal under the terms of Creative Commons Attribution License, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this Journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form of which it has been published by the Journal (for example, to upload the work to the online storage of the Journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this Journal is included.