Original article
Ukrainian Neurosurgical Journal. 2025;31(2):75-85
https://doi.org/10.25305/unj.325159
Department of Neurosurgery, Smt. NHL Municipal Medical College and Sardar Vallabhbhai Patel Institute of Medical Sciences and Research, Ahmedabad, Gujarat, India
Received: 20 March 2025
Accepted: 07 May 2025
Address for correspondence:
Shreyansh Patel, Department of Neurosurgery, Smt. NHL Municipal Medical College and Sardar Vallabhbhai Patel Institute of Medical Sciences and Research, Ahmedabad 380006, Gujarat, India, e-mail: shreyanshpatel1110@gmail.com
Aim: This prospective observational study was done to evaluate the outcomes and management of patients with degenerative cervical myelopathy (DCM) treated with anterior cervical discectomy and fusion (ACDF).
Materials and methods: Our study included 80 patients with DCM admitted to a neurosurgical department between August 2013 and February 2023. Patients underwent ACDF surgery for single- or multi-level spinal canal stenosis. Demographic data, clinical features, and neurological examinations including assessments of limb power using the Medical Research Council Scale, sensory system function, and sphincter disturbance pre- and post-operatively were assessed. Pre- and post-operative neurological function was evaluated using the Nurick score, while post-operative outcomes were assessed using the Odom's criteria. The study population consisted mainly of males aged 51-60 years. Myelopathy was the most frequent presentation, with C5-C6 level being the most common level of fusion.
Results: ACDF surgery significantly improved neurological function, as evidenced by reduced pre-operative weakness and sensory dysfunction, and increased post-operative muscle strength. Minimal postoperative complications were observed.
Conclusions: These findings align with previous research, demonstrating ACDF as a safe and effective procedure for improving neurological function and quality of life in DCM patients. Limitations include sample size and study design, necessitating further research.
Key words: degenerative cervical myelopathy; anterior cervical discectomy and fusion; myeloradiculopathy; Nurick score; Odom's criteria
Introduction
Degenerative cervical myelopathy (DCM) represents the most prevalent cause of spinal cord impairment among adults globally [1]. This clinicopathological entity encompasses a broad spectrum of acquired and congenital conditions, including degenerative changes, hypertrophy, and calcification of the intervertebral discs, ligaments, and bony structures of the cervical spine. Notable examples include cervical spondylosis and ossification of the posterior longitudinal ligament (OPLL) [2,3]. These pathological processes result in stenosis of the cervical spinal canal, leading to chronic compression of the spinal cord and subsequent neurological and functional disabilities [4]. Cervical degenerative disc disease can be particularly debilitating, significantly compromising the quality of life. Magnetic Resonance Imaging (MRI) studies have demonstrated that many adults may present with cervical degenerative disc disease without exhibiting any clinical symptoms [5,6]. For symptomatic patients, conservative management is generally the initial preferred approach, with the majority responding positively to such treatment [7]. However, anterior cervical discectomy and fusion (ACDF) is recommended for patients who do not respond to conservative management [8-12]. In a well-selected cohort of patients characterized by younger age, a single-level soft disc, male gender, non-smokers, congruent radiological and clinical findings, and well-preserved neurological function, ACDF has been associated with favourable outcomes [13,14]. In this study, we evaluated the clinical presentations and outcomes following ACDF in patients with cervical degenerative disc disease across various age groups.
Aim and objectives
Aim:
To evaluate the outcomes and management of patients with degenerative cervical myelopathy treated with ACDF.
Objectives:
Materials and methods
This prospective observational study was conducted at a single tertiary care hospital, focusing on patients admitted with degenerative cervical myelopathy to the Department of Neurosurgery from August 2013 to February 2023. Consent was obtained from all participants. A total of 80 patients were included in the study. The inclusion criteria encompassed patients presenting with cervical compressive myelopathy and myeloradiculopathy, affected at spinal levels between C3 and C7, with myelopathy secondary to cervical spinal canal stenosis involving the disc, patients experiencing persistent complaints unresponsive to conservative management for a minimum of three months, and those diagnosed with posterior osteophyte complex disease. Exclusion criteria included patients with cervical trauma, age less than 18 years, ongoing cervical infection and inflammation, and those presenting solely with radiculopathy. Baseline demographic data including age, sex, and medical history were collected. Clinical features, presenting symptoms, duration of symptoms, and neurological examination findings were documented. Pre-operative imaging studies, including X-ray of cervical spine antero-posterior and lateral views, MRI of cervical spine with whole spine screening were done. All surgeries were performed by experienced neurosurgeons using standardized techniques for ACDF. Intraoperative data, including the level of fusion, number of fusions and any intraoperative complications, were recorded. Clinical examinations were conducted at periodic intervals post-surgery (during the hospital stay, at the first follow-up during suture removal, and at three, six, and twelve months). During these examinations patients were asked whether their symptoms were the same, better, or worse post-surgery. At the six-month follow-up, patients were assessed based on Odom's criteria (excellent: no complaints and able to carry out physical activities; good: minimal persistence of preoperative symptoms but physical activities possible without significant interference; fair: relief of some preoperative symptoms with significant limitation in physical activities; poor: worsened or unchanged symptoms and signs) Patients were also assessed using the Nurick score (Grade 0: no root or cord symptoms; Grade I: root signs or symptoms with no cord involvement; Grade II: signs of cord involvement with normal gait; Grade III: gait abnormality but able to be employed; Grade IV: gait abnormality prevents employment; Grade V: able to ambulate only with assistance; Grade VI: chair-bound or bedridden). There were no cases of loss to follow-up.
Results
Table 1 summarises demographic details (age and gender distribution) and clinical characteristics of patients (clinical symptoms and duration of symptoms) diagnosed with cervical degenerative myelopathy.
Table 1. Demographic and clinical characteristics of patients with cervical degenerative myelopathy
|
Characteristic |
Number of patients |
Percentage |
|
Age distribution (years) |
||
|
21-30 |
2 |
2.5% |
|
31-40 |
9 |
11.25% |
|
41-50 |
28 |
35% |
|
51-60 |
37 |
46.25% |
|
61-70 |
4 |
5% |
|
Gender distribution |
||
|
Male |
66 |
82.50% |
|
Female |
14 |
17.50% |
|
Duration of symptoms |
||
|
<6 months |
29 |
36.25% |
|
6-12 months |
42 |
52.5% |
|
>12 months |
9 |
11.25% |
|
Clinical symptoms |
||
|
Myelopathy |
63 |
78.75% |
|
Myeloradiculopathy |
17 |
21.25% |
The age distribution of patients reveals a predominant occurrence in the age group of 51-60 years, comprising 37 patients (46.25%) of the study population, followed by those aged 41-50 years with 28 patients (35%). Gender distribution shows a higher prevalence among males, accounting for 66 patients (82.50%). The duration of symptoms varied, with a notable proportion of patients, 42 (52.5%) reporting symptom durations between 6 to 12 months. Clinical symptoms observed in the patients include myelopathy, affecting 63 patients (78.75%) of the study population, and myeloradiculopathy, observed in 17 patients (21.25%).
Table 2 summarises the level of ACDF and the number of fusion procedures performed. It reveals that the majority of patients underwent single-level ACDF fusion surgery, with 67 patients receiving this intervention. Twelve patients underwent double-level fusion, and one patient underwent a three-level fusion in a single sitting.
Table 2. Surgical intervention details
|
Level of ACDF fusion |
Number of patients |
|
C3-C4 |
22 |
|
C4-C5 |
22 |
|
C5-C6 |
38 |
|
C6-C7 |
12 |
|
Number of fusions |
|
|
Single-level ACDF fusion |
67 |
|
Double-level ACDF fusion |
12 |
|
Three-level ACDF fusion |
1 |
|
Note: ACDF - Anterior cervical discectomy and fusion |
|
Table 3 shows neurological examination preoperatively and postoperatively in the form of an assessment of limb power on the Medical Research Council (MRC) scale, sensory system examination, sphincter disturbances and surgical complications. Pre-operative power grades varied, with the majority, 39 patients (48.75%) falling into grade 4-, while post-operative assessments showed significant improvements, particularly in grades 4 and 4+. Sensory system evaluations revealed sensory affection in 28 patients (35%) pre-operatively, with a significant improvement noted post-operatively. Sphincter disturbance, specifically bladder involvement, was present in ten patients (12.50%) pre-operatively, of which two patients had improved sphincter control while the remaining eight patients (10%) showed no change post-operatively. Regarding complications, no intraoperative complications were reported, while three patients (6.3%) experienced immediate postoperative complications, primarily characterized by limb weakness and five patients (6.25%) experienced delayed postoperative complications in the form of non-improvement of symptoms of pain and spasticity. Complications such as severe blood loss, dysphagia, oesophageal perforation, infections, vocal cord palsy, and kyphosis, were not observed in this study.
Table 3. Neurological examination pre- and post-operatively and complications
|
Evaluation |
Number of patients (percentage) |
|
|
Preoperative |
Postoperative |
|
|
Limb Power (MRC Scale) |
||
|
Grade 3 |
12 (15%) |
6 (7.50%) |
|
Grade 4- |
39 (48.75%) |
8 (10%) |
|
Grade 4 |
29 (36.25%) |
40 (50%) |
|
Grade 4+ |
0 |
26 (32.50%) |
|
Sensory system examination |
||
|
Affected |
28 (35%) |
16 (20%) |
|
Non-affected |
52 (65%) |
64 (80%) |
|
Sphincter disturbance |
||
|
Present |
10 (12.50%) |
8 (10%) |
|
Absent |
70 (87.50%) |
72 (90%) |
|
Surgical complications |
||
|
Intraoperative |
0 |
|
|
Immediate postoperative |
3 (3.75%) |
|
|
Delayed postoperative |
5 (6.25%) |
|
|
Note: MRC - Medical Research Council |
||
Table 4 summarises Nurick score evaluation conducted pre-operatively and post-operatively and the outcome assessment based on Odom's criteria. Nurick score evaluation indicates improvements in neurological function following surgical intervention. The distribution of Nurick score post-operatively shows a decrease in scores compared to pre-operative assessments. Outcome assessment based on Odom's criteria demonstrates that the majority of patients, 31 (38.75%) achieved excellent outcomes, followed by a good outcome in 27 patients (33.75%), a fair outcome in 17 patients (21.25%) and a poor outcome in 05 patients (6.25%), reflecting positive outcomes in terms of neurological improvement post-surgery.
Table 4. Nurick score evaluation preoperatively and postoperatively and Odom's criteria outcome assessment
|
Evaluation |
Number of patients |
|
|
Preoperative |
Postoperative |
|
|
Nurick score |
||
|
0 |
0 |
16 |
|
1 |
0 |
29 |
|
2 |
30 |
21 |
|
3 |
35 |
9 |
|
4 |
9 |
5 |
|
5 |
6 |
0 |
|
Odom's criteria outcome |
Number of patients |
|
|
Excellent |
31 (38.75%) |
|
|
Good |
27 (33.75%) |
|
|
Fair |
17 (21.25%) |
|
|
Poor |
5 (6.25%) |
|
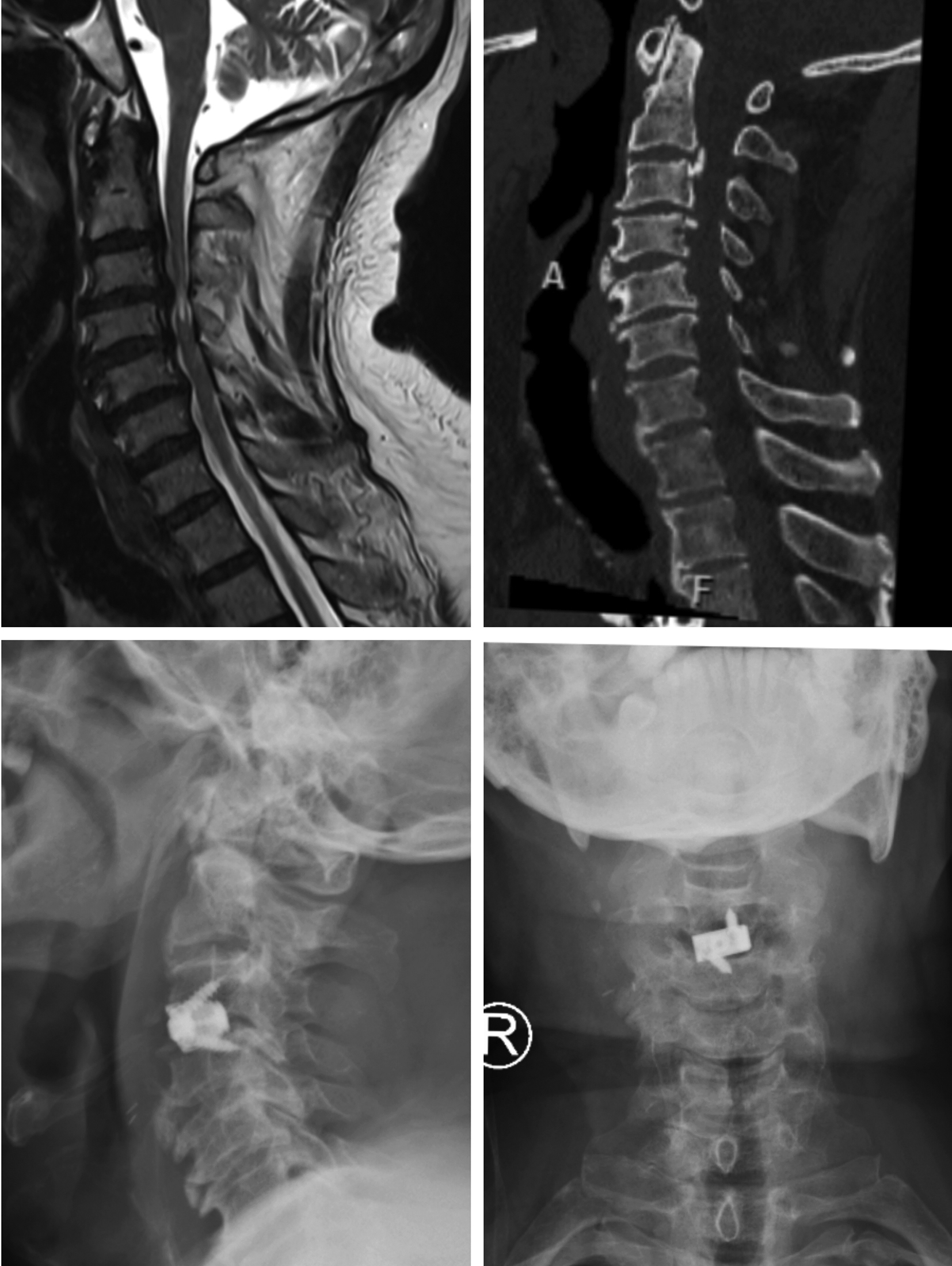
Figures 1-4 show pre-operative and post-operative radiological images in few of our patients.
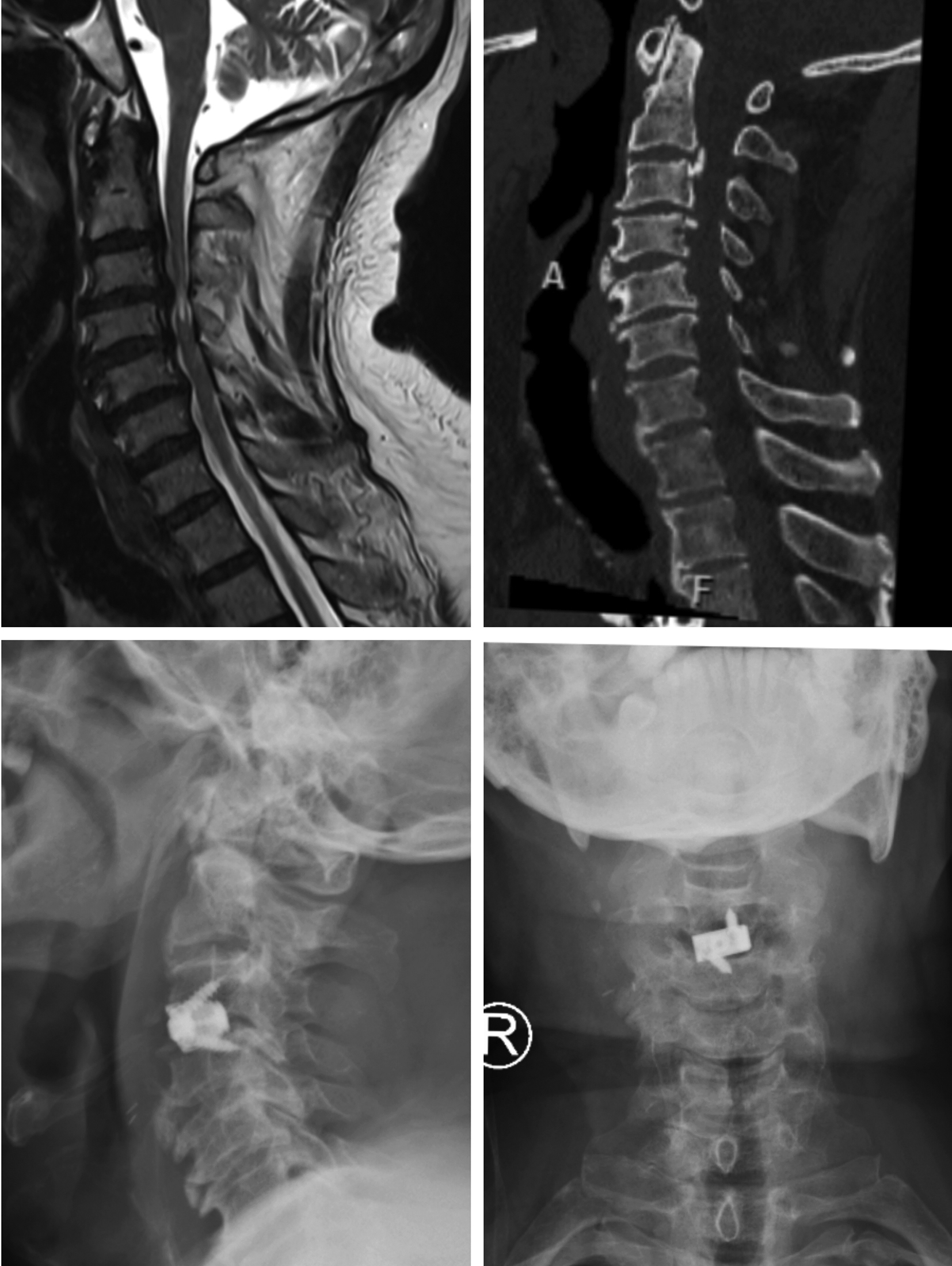
Figure 1. A - Preoperative magnetic resonance imaging study of the cervical spine, (T2 weighted image, sagittal view) showing narrowing of central canal with cervical compressive myelopathy; B - Preoperative computed tomography imaging study of the cervical spine (sagittal view) showing osteophytes with narrowing of the central canal and straitening of the cervical lordosis; C - Postoperative radiographic imaging study of the cervical spine (sagittal view) showing the cage with screw in situ; D - Postoperative radiographic imaging study of the cervical spine (coronal view) showing the cage with screw in situ

Figure 2. A - Preoperative magnetic resonance imaging study of the cervical spine (T2 weighted image, sagittal view) showing cervical compressive myelopathy with disc osteophyte complex; B - Postoperative radiographic imaging study of the cervical spine (sagittal view) showing the cage in situ; C - Postoperative radiographic imaging study of the cervical spine (coronal view) showing the cage in situ

Figure 3. A - Preoperative magnetic resonance imaging study of the cervical spine (T2 weighted image, sagittal view) showing cervical compressive myelopathy with disc osteophyte complex; B - Postoperative radiographic imaging study of the cervical spine (sagittal view) showing the cage in situ; C - Postoperative radiographic imaging study of the cervical spine (coronal view) showing the cage in situ
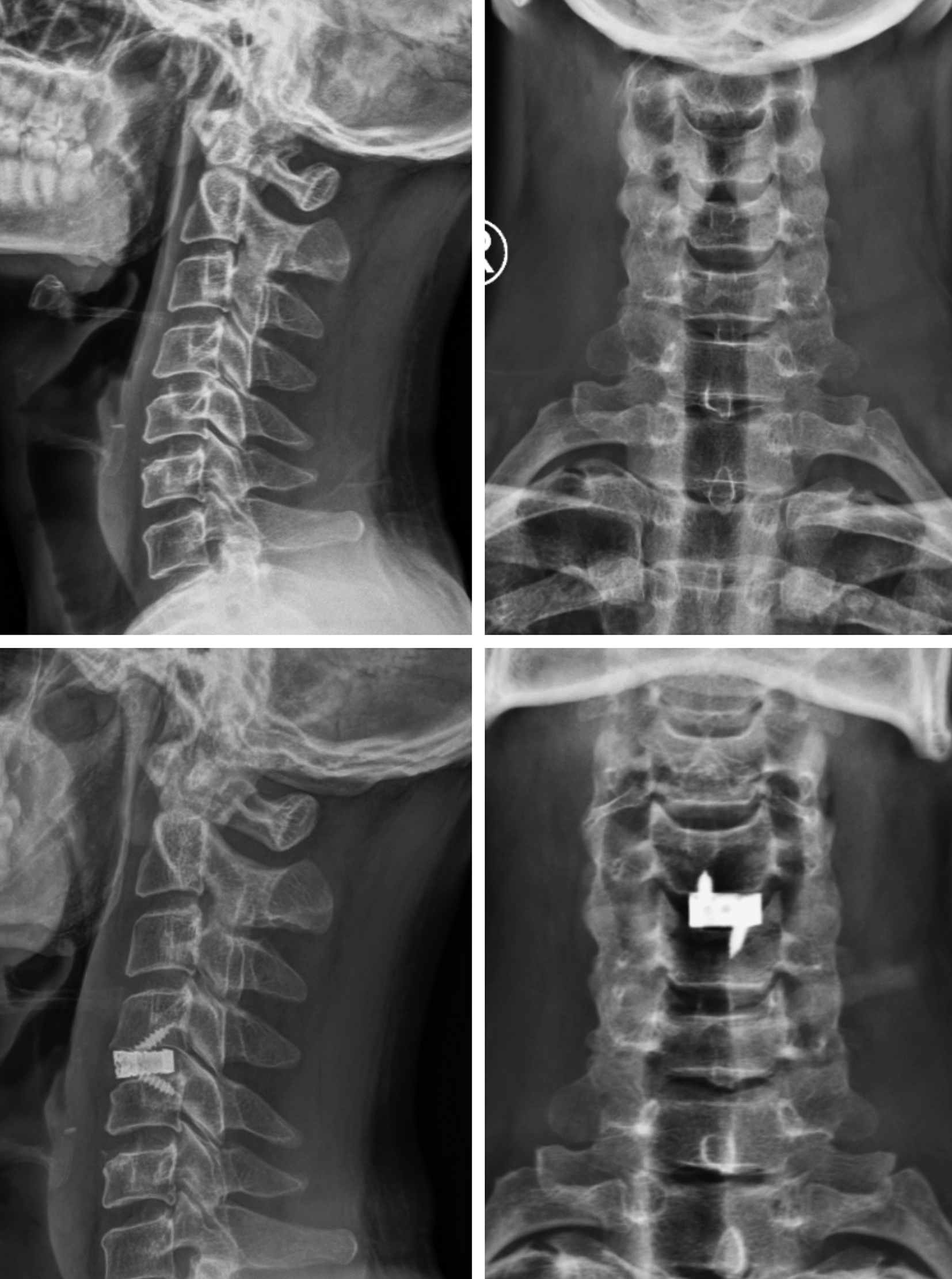
Figure 4. A - Preoperative radiographic imaging study of the cervical spine (sagittal view) showing disc-osteophyte complex causing narrowing of the central canal; B - Preoperative radiographic imaging study of the cervical spine (coronal view); C - Postoperative radiographic imaging study of the cervical spine (sagittal view) showing the cage with screw in situ; D - Postoperative radiographic imaging study of the cervical spine (coronal view) showing the cage with screw in situ
Discussion
DCM is a significant condition that has garnered considerable research attention, with the aim of deepening our understanding of its pathophysiology and management. Key anatomical structures commonly affected by DCM include the vertebral body, intervertebral discs, posterior longitudinal ligament, ligamentum flavum, and uncovertebral joints. The clinical presentation of DCM may encompass motor, sensory, and/or sphincter dysfunction, often accompanied by notable signs such as Hoffman's sign and the inverted brachioradialis reflex. Diagnosis is primarily established through a clinical examination, supported by MRI evidence of cord compression [15]. The Nurick score remains a critical tool in evaluating neurological function both before and after surgical intervention. Surgical management is the cornerstone of DCM treatment, with approaches varying between anterior, posterior, or a combination of both. The anterior approach, including procedures such as corpectomy or ACDF, is generally preferred due to its association with fewer complications and a shorter hospital stay [3, 4]. Since the introduction of ACDF in 1958 [12] it has become one of the most frequently performed spinal surgeries [16]. ACDF is widely regarded as the gold standard for addressing degenerative cervical spine diseases due to its relatively low risk profile, reproducibility, and reliability [17]. A meta-analysis by Shahab Aldin Sattari et al. [18] found no significant differences between ACDF and posterior decompression in terms of functional outcomes at the one-year follow-up. However, ACDF was associated with less intraoperative bleeding, shorter hospital stays, and lower rates of surgical site infections and C5 palsy.
Our study focused on the outcomes of surgical interventions for degenerative cervical myelopathy/myeloradiculopathy in 80 patients. The findings revealed a predominance of the condition in middle-aged males, with the most affected age group being 51-60 years, accounting for 46.25% of the cases, followed by the 41-50 years age group, representing 35% of the cases. Gender distribution demonstrated a higher prevalence among males (82.50%) compared to females (17.50%). These demographic details are consistent with the studies conducted by Shrikhande N.N. et al. [19] and Saravanan A et al. [20]. Several clinical syndromes are associated with cervical disc disease including cervical spondylotic myelopathy/ myeloradiculopathy, cervical radiculopathy, and neck pain syndromes. Our study excluded cases involving only radiculopathy or neck pain syndrome, focusing primarily on patients presenting with myelopathy (78.75%) or mixed symptoms of myeloradiculopathy (21.25%), aligning with the observations of Shrikhande N.N. et al. [19] and Hwang et al. [21]. Furthermore, approximately 52.5% of the patients reported symptoms lasting 6 to 12 months, similar to findings by Suri A. et al. [22]. However, Ramesh et al. [23] highlighted a significant proportion of patients experiencing symptoms for over 12 months, underscoring the importance of early detection and prompt intervention to optimize outcomes and prevent further neurological deterioration.
In terms of surgical procedures, the most frequently observed single-level of fusion was at C5-C6, occurring in 38 cases, consistent with Shrikhande N.N. et al. [19] and Saravanan A. et al. [20]. Double-level fusion surgery was performed on 12 patients, with only one patient undergoing three-level fusion in a single sitting, further aligning with the findings of Shrikhande N.N. et al. [19] and Saravanan A. et al. [20], indicating that three-level fusion is less frequently performed.
Our analysis revealed significant improvements in neurological function following surgery. Pre-operative weakness Grade 4- MRC scale decreased substantially from 48.75% to 10% postoperatively, accompanied by a notable increase in excellent muscle strength Grade 4+ MRC scale from 0% to 32.50%. Additionally, pre-operative sensory dysfunction decreased from 35% to 20% post-surgery. The rate of sphincter disturbances remained consistent at around 10% pre- and post-operatively, similar to the findings of Shrikhande N.N. et al. [19] who reported no significant improvement in this area. Although the study was limited by sample size and design, the minimal postoperative surgical complications (3.75% immediate, 6.25% delayed) suggest ACDF as a safe and effective procedure for improving neurological function in DCM patients. The postoperative weakness was also improved gradually in all the patients. In contrast, studies by Mastronardi L. et al. [24] and Choi S.H. et al. [25] reported various complications, including severe blood loss, dysphagia, oesophageal perforation, infections, vocal cord palsy, and kyphosis. None of these were observed in our study. This absence of severe complications suggests successful surgical management and perioperative care, contributing to favourable outcomes.
The mean preoperative Nurick score, indicating the severity of impairment, was 2.57. However, this score improved significantly post-surgery, dropping to 1.12 on average. Consistent with these findings, studies by Gupta A. et al. [26] demonstrated significant reductions in Nurick scores after surgery, further supporting the notion that ACDF intervention can lead to reduced neurological impairment and enhanced functional abilities in DCM patients. The decrease in postoperative Nurick scores across these studies suggests that surgical treatment plays a crucial role in enhancing patients’ quality of life and functional abilities. Furthermore, analysis using Odom's criteria at six months revealed positive outcomes for a substantial portion of patients. Nearly 40% (38.75%) achieved an excellent outcome, with good and fair outcomes were observed in an additional 55% of patients. These results are comparable to previous research by Hassan M. et al. [27] and Saravanan A. et al. [20], who also reported high rates of positive outcomes following ACDF surgery for DCM. While limitations including sample size and study design necessitate further research involving larger, controlled studies, the current findings provide promising evidence of the effectiveness of ACDF surgery in improving outcomes for DCM patients. Additionally, the study by Long Tang et al. [28] suggests that day-surgery ACDF may offer safety and early efficacy comparable to traditional inpatient procedures, presenting a promising alternative for eligible patients. This research highlights the potential of ACDF surgery to improve neurological function and functional abilities, ultimately enhancing patients’ quality of life.
Conclusion
Our study investigated the effectiveness of ACDF surgery in managing DCM in 80 patients. Our analysis revealed a predominance of the condition in middle-aged males, with the most frequent surgical level being C5-C6. Significantly, ACDF surgery resulted in substantial improvements in neurological function, as evidenced by reductions in pre-operative weakness and sensory dysfunction, along with a notable increase in excellent muscle strength. Furthermore, the minimal postoperative complications observed suggest ACDF as a safe and effective procedure for patients with DCM. The study also highlights the importance of early intervention. These findings align with previous research demonstrating positive outcomes following ACDF surgery. The decrease in Nurick scores across our study and others highlights the potential of ACDF intervention to improve neurological function, functional abilities, and ultimately, patient quality of life in DCM patients. While limitations including sample size and study design necessitate further research with larger, controlled studies, the current results provide promising evidence for the effectiveness of ACDF surgery in managing DCM.
Declarations
Disclosure
Hereby it is stated that the manuscript has been read and approved by all the authors. Each author believes affirms that the manuscript represents honest work and confirms that the information has not been published or submitted elsewhere in any form.
Consent
Informed consent was obtained from all participants.
Conflict of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Funding
The authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
Author’s contribution
All authors contributed equally to the manuscript and approved the final version of the manuscript.
Research ethics
This study was observational, focusing on patients with Degenerative cervical myelopathy (DCM). All participants received the same standard treatment. The study aimed to evaluate the outcomes and management of patients with degenerative cervical myelopathy treated with ACDF. Objectives were to determine the age- and sex-specific incidence of cervical degenerative disease in the study population, to assess the clinical features, outcomes, and complications associated with cervical degenerative disease in patients treated with ACDF and to compare pre-operative and post-operative Nurick scores as well as postoperative Odom's criteria outcomes without any deviation from standard clinical practice.
Given that the study was purely observational and did not involve any experimental procedures, manipulation of variables, or assignment of participants to different treatment groups, it was deemed to fall under the category of research that does not require IRB approval. All data were collected in a manner consistent with routine clinical practice, ensuring that patient care was not impacted in any way by the study. Patient confidentiality and ethical standards were strictly maintained throughout the study. No identifiable patient information was collected, and all data were anonymized to protect the privacy of the participants.
References
1. Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87-100. https://doi.org/10.1093/brain/95.1.87
2. Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative Cervical Myelopathy: Epidemiology, Genetics, and Pathogenesis. Spine (Phila Pa 1976). 2015 Jun 15;40(12):E675-93. https://doi.org/10.1097/BRS.0000000000000913
3. Badhiwala JH, Ahuja CS, Akbar MA, Witiw CD, Nassiri F, Furlan JC, Curt A, Wilson JR, Fehlings MG. Degenerative cervical myelopathy - update and future directions. Nat Rev Neurol. 2020 Feb;16(2):108-124. https://doi.org/10.1038/s41582-019-0303-0
4. Karadimas SK, Erwin WM, Ely CG, Dettori JR, Fehlings MG. Pathophysiology and natural history of cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2013 Oct 15;38(22 Suppl 1):S21-36. https://doi.org/10.1097/BRS.0b013e3182a7f2c3
5. de Bruin F, Ter Horst S, van den Berg R, de Hooge M, van Gaalen F, Fagerli KM, Landewé R, van Oosterhout M, Bloem JL, van der Heijde D, Reijnierse M. Signal intensity loss of the intervertebral discs in the cervical spine of young patients on fluid sensitive sequences. Skeletal Radiol. 2016 Mar;45(3):375-81. https://doi.org/10.1007/s00256-015-2301-7
6. Teraguchi M, Yoshimura N, Hashizume H, Muraki S, Yamada H, Minamide A, Oka H, Ishimoto Y, Nagata K, Kagotani R, Takiguchi N, Akune T, Kawaguchi H, Nakamura K, Yoshida M. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthritis Cartilage. 2014 Jan;22(1):104-10. https://doi.org/10.1016/j.joca.2013.10.019
7. Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994 Apr;117 ( Pt 2):325-35. https://doi.org/10.1093/brain/117.2.325
8. Jacobs W, Willems PC, van Limbeek J, Bartels R, Pavlov P, Anderson PG, Oner C. Single or double-level anterior interbody fusion techniques for cervical degenerative disc disease. Cochrane Database Syst Rev. 2011 Jan 19;(1):CD004958. https://doi.org/10.1002/14651858.CD004958.pub2
9. Cepoiu-Martin M, Faris P, Lorenzetti D, Prefontaine E, Noseworthy T, Sutherland L. Artificial cervical disc arthroplasty: a systematic review. Spine (Phila Pa 1976). 2011 Dec 1;36(25):E1623-33. https://doi.org/10.1097/BRS.0b013e3182163814
10. CLOWARD RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958 Nov;15(6):602-17. https://doi.org/10.3171/jns.1958.15.6.0602
11. ROBINSON RA. Fusions of the cervical spine. J Bone Joint Surg Am. 1959 Jan;41-A(1):1-6.
12. SMITH GW, ROBINSON RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958 Jun;40-A(3):607-24.
13. Anderson PA, Subach BR, Riew KD. Predictors of outcome after anterior cervical discectomy and fusion: a multivariate analysis. Spine (Phila Pa 1976). 2009 Jan 15;34(2):161-6. https://doi.org/10.1097/BRS.0b013e31819286ea
14. Peolsson A, Peolsson M. Predictive factors for long-term outcome of anterior cervical decompression and fusion: a multivariate data analysis. Eur Spine J. 2008 Mar;17(3):406-414. https://doi.org/10.1007/s00586-007-0560-2
15. Saunders LM, Sandhu HS, McBride L, Maniarasu VS, Taylor S, Dhokia R. Degenerative Cervical Myelopathy: An Overview. Cureus. 2023 Dec 12;15(12):e50387. https://doi.org/10.7759/cureus.50387
16. Saifi C, Fein AW, Cazzulino A, Lehman RA, Phillips FM, An HS, Riew KD. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J. 2018 Jun;18(6):1022-1029. https://doi.org/10.1016/j.spinee.2017.10.072
17. Fowler SB, Anthony-Phillips P, Mehta D, Liebman K. Health-related quality of life in patients undergoing anterior cervical discectomy fusion. J Neurosci Nurs. 2005 Apr;37(2):97-100.
18. Sattari SA, Ghanavatian M, Feghali J, Rincon-Torroella J, Yang W, Xu R, Bydon A, Witham T, Belzberg A, Theodore N, Lubelski D. Anterior cervical discectomy and fusion versus posterior decompression in patients with degenerative cervical myelopathy: a systematic review and meta-analysis. J Neurosurg Spine. 2023 Feb 24:1-13. https://doi.org/10.3171/2023.1.SPINE221244
19. Srikhande NN, Kumar VAK, Sai Kiran NA, Ghosh A, Pal R, Moscote-Salazar LR, Kumar VA, Reddy VV, Agrawal A. Clinical presentation and outcome after anterior cervical discectomy and fusion for degenerative cervical disc disease. J Craniovertebr Junction Spine. 2019 Jan-Mar;10(1):28-32. https://doi.org/10.4103/jcvjs.JCVJS_87_18
20. Saravanan A, Ismail ND, Kumar SM, Rajarajan E, Anandan H. Functional and Radiological Outcome Analysis of Anterior Cervical Discectomy and Fusion in Cervical Spondylotic Myeloradiculopathy. International Journal of Scientific Study. 2017;5(4):155-7.
21. Hwang SL, Lee KS, Su YF, Kuo TH, Lieu AS, Lin CL, Howng SL, Hwang YF. Anterior corpectomy with iliac bone fusion or discectomy with interbody titanium cage fusion for multilevel cervical degenerated disc disease. J Spinal Disord Tech. 2007 Dec;20(8):565-70. https://doi.org/10.1097/BSD.0b013e318036b463
22. Suri A, Chabbra RP, Mehta VS, Gaikwad S, Pandey RM. Effect of intramedullary signal changes on the surgical outcome of patients with cervical spondylotic myelopathy. Spine J. 2003 Jan-Feb;3(1):33-45. https://doi.org/10.1016/s1529-9430(02)00448-5
23. Ramesh VG, Kannan MGV, Sriram K, Balasubramanian C. Prognostication in cervical spondylotic myelopathy: Proposal for a new simple practical scoring system. Asian J Neurosurg. 2017 Jul-Sep;12(3):525-528. https://doi.org/10.4103/1793-5482.146391
24. Mastronardi L, Ducati A, Ferrante L. Anterior cervical fusion with polyetheretherketone (PEEK) cages in the treatment of degenerative disc disease. Preliminary observations in 36 consecutive cases with a minimum 12-month follow-up. Acta Neurochir (Wien). 2006 Mar;148(3):307-12; discussion 312. https://doi.org/10.1007/s00701-005-0657-5
25. Choi SH, Kang CN. Degenerative Cervical Myelopathy: Pathophysiology and Current Treatment Strategies. Asian Spine J. 2020 Oct;14(5):710-720. https://doi.org/10.31616/asj.2020.0490
26. Gupta A, Rajshekhar V. Functional and radiological outcome in patients undergoing three level corpectomy for multi-level cervical spondylotic myelopathy and ossified posterior longitudinal ligament. Neurol India. 2016 Jan-Feb;64(1):90-6. https://doi.org/10.4103/0028-3886.173654
27. Mohammed H, Khalaf MA, El Khayat RA. Evaluation of Different Modalities of Anterior Cervical Discectomy for Treatment of Single and Double Level Cervical Disc Herniation. Open Access Journal of Neurology & Neurosurgery. 2018;8(5):83-94. https://doi.org/10.19080/OAJNN.2018.08.555748
28. Tang L, Chen Y, Wang F, Liu Y, Song Z, Wang M, Zhou Y, Liu H, Zheng J. Safety and efficacy of day anterior cervical discectomy and fusion procedure for degenerative cervical spondylosis: a retrospective analysis. BMC Musculoskelet Disord. 2024 Mar 19;25(1):223. https://doi.org/10.1186/s12891-024-07356-7