Original article
Ukrainian Neurosurgical Journal. 2025;31(2):69-74
https://doi.org/10.25305/unj.325120
1 Department of Neurosurgery, NRSMCH, Kolkata, West Bengal, India
2 Department of Anaesthesia, AIIMS Patna, Bihar, India
Received: 20 March 2025
Accepted: 25 April 2025
Address for correspondence:
Anita Singh, Department of Anaesthesia, All India Institute of Medical Sciences Patna, Phulwarisharif, Patna, Bihar,-801507, India, e-mail:anitajiwesh@gmail.com
Lumbar disc herniation is a prevalent spinal condition characterized by the displacement of intervertebral disc material leading to back pain and neuropathies. Surgical intervention, including decompressive laminectomy, is often recommended for patients who fail to respond to conservative treatment. The procedure of unilateral or bilateral lower half laminectomy, with or without disc herniation removal, has been described as an effective surgical technique for treating lumbar disc herniations.
Purpose: The aim of the study was the assessment of outcomes including complications in patients undergoing limited laminectomy with discectomy.
Material and methods: A total of 188 patients over a period from May 2022 till May 2024 were prospectively studied.Outcomes were assessed using Odom’s criteria, including complication, recovery status at subsequent follow up at 1 and 3 months.
Results: Out of 188 patients, single disc herniations were seen in 155 while 2-level disc were seen in 33 cases. Among these, L5-S1 level herniation was most common , and in multi-disc herniation, L5-L5,L5-S1 levels were common. Most patients presented with radicular pain(127) followed by motor deficits or sensory deficits. Post operative recovery status was classified as excellent in the majority of cases (121 out of 188) with very less in fair and none in poor category. The recovery was gradually towards better grades in subsequent follow-ups. Duration of surgery was less than 1 hour in about 90% cases (16 out of 188).
Conclusions: All cases were done under spinal anaesthesia. Adequate surgical exposure was obtained. The technique allowed for early mobilization, reduced hospital stay apart from a shorter learning curve requirement as compared to microscopic or endoscopic procedures. During discectomy the thickened ligamentum flavum (causing canal stenosis/narrowing) can also be dealt in single procedure. This procedure could be a safer alternative to the newer modalities of minimally invasive surgeries for lumbar decompression.
Keywords: limited laminectomy; open decompression; disc herniation
Introduction
Lumbar disc herniation is a prevalent spinal condition characterized by the displacement of intervertebral disc material, frequently resulting in significant back and leg discomfort, and in severe instances, neurological impairments such as weakness, numb sensations, and bladder/bowel dysfunction [1]. Surgical intervention, including decompressive laminectomy, is often recommended for patients who fail to respond to conservative treatments or those with severe or progressive neurological deficits [2]. While open surgical procedures have traditionally been the standard approach, in recent years, minimally invasive surgical techniques have gained popularity due to their potential benefits, such as reduced surgical trauma, shorter hospital stays, and faster recovery times [3].
One such minimally invasive technique is the lower half laminectomy, which involves the removal of the inferior portion of the lamina to access and decompress the affected spinal level [4]. At our institute, single-level or double -level discectomies without fixation are usually administered under spinal anaesthesia unless the patient specifically refuses or there is any high risk/ comorbidities associated,thereby prohibiting the use. In this case series, all procedures which were done under spinal anesthesia have been retrospectively studied from May 2022 till May 2024.
The procedure of unilateral or bilateral lower half laminectomy, with or without disc herniation removal, has been described as an effective surgical technique for treating lumbar disc herniations. Performing these lower half laminectomies under spinal anesthesia, rather than general anesthesia, confers several advantages while post operative complication rates are comparable to that associated with microdisscectomies or endoscopic procedures etc. and also avoiding complications related to general anaesthesia.
Purpose: The aim of the study was the assessment of outcomes including complications in patients undergoing limited laminectomy with discectomies.
Materials and methods
Type of study:
Prospective cohort study
Study duration:
May 2022- May 2024
Study location:
Department of Neurosurgery, NRSMCH, Kolkata.
Study population:
All subsequently admitted patients undergoing single or double level limited laminectomy and discestomies/ decompression without fixation under spinal anaesthesia.
Exclusion criteria:
Patients with severe canal stenosis accompanied by facet arthropathy, any radiologic evidence of subluxation, or multilevel involvement (more than three levels) were excluded from the study( as they required more extensive decompression with or without fusion/fixation). Prior to any surgical intervention, patients underwent clinical assessment, MRI, and dynamic X-rays of the lumbosacral spine. Postoperative evaluations were carried out according to Odom’s criteria (Culloch, 1996) [5].
Sample size:
A total of 188 patients were studied.
All cases were conducted in the prone position under spinal anesthesia using a Bupivacaine/Fentanyl mixture.
Details of the Operative Procedure:
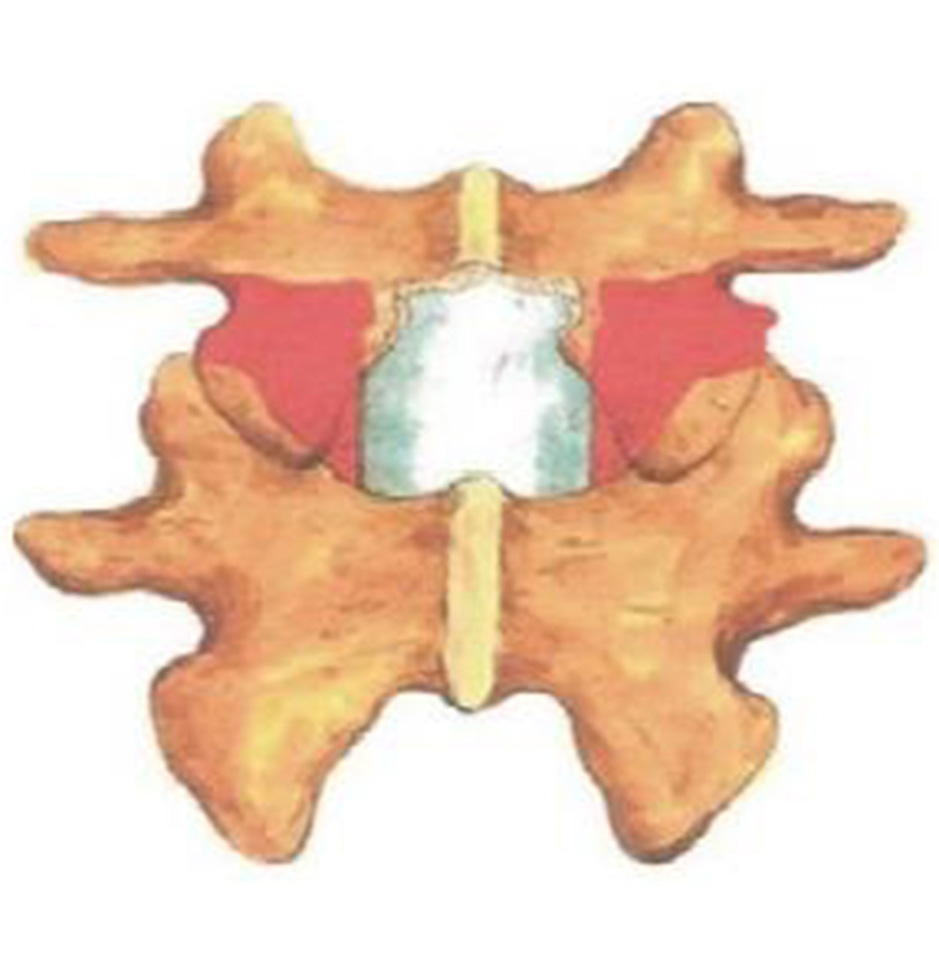
Following spinal anesthesia, patients were positioned prone. A midline incision was made one level above and below the involved segment. C-arm intensifier was utilized, especially when sacralization or lumbarization was identified in preoperative imaging. The spine and laminae were exposed, centering on the affected disc space. Portions of the spinous process and interspinous ligament were excised. The lower halves of both laminae were removed until the epidural fat became visible through the ligamentum flavum in the midline. (Fig. 1). The ligamentum flavum was excised bilaterally, and in certain cases, the overhanging portions of the hypertrophied medial facets were removed using a Kerrison punch. A standard technique was employed for discectomy, ensuring the complete removal of all visible disc material. Both nerve roots were examined for any additional compressive elements before they entered their respective foramina. For L5-S1 disc prolapse, only ligamentum flavectomy was performed with limited laminectomy (even less than the lower half) to facilitate adequate discectomy. The wounds were closed in layers after achieving proper hemostasis. For illustration images from a case of L5-S1 disc prolapsed are presented(pre-operative MRI and post operative X-ray) (Fig. 2-4).
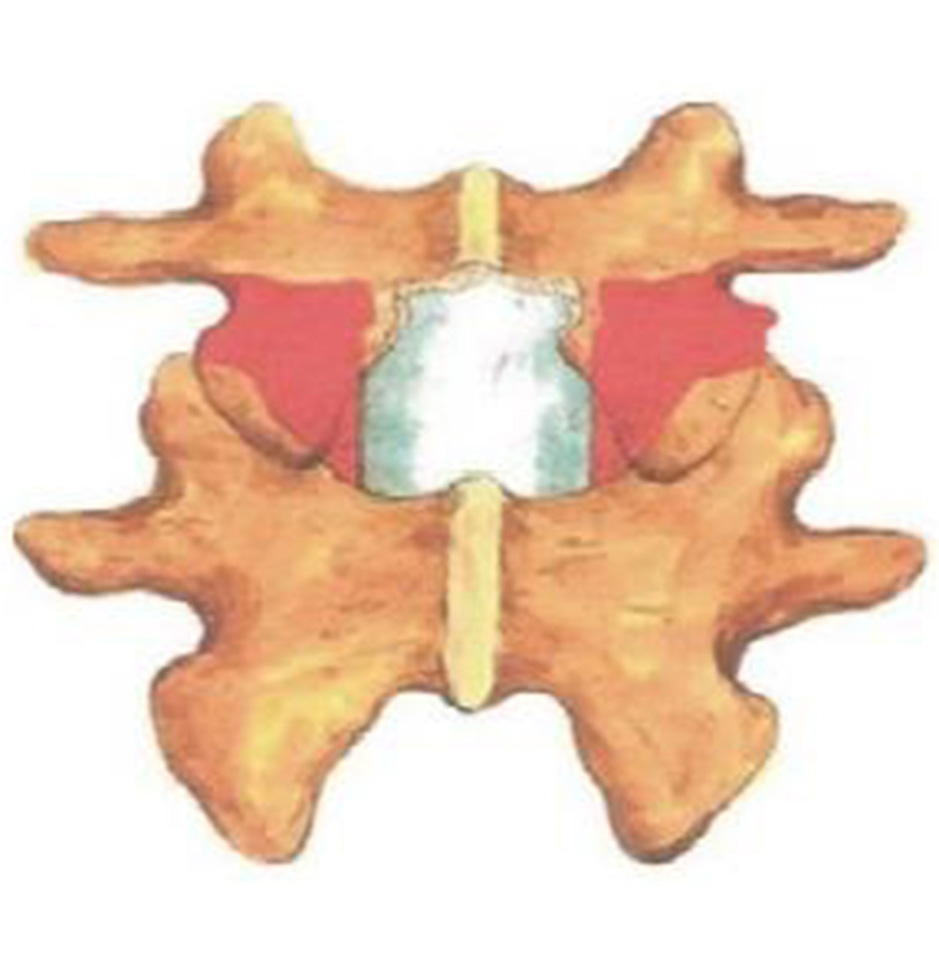
Fig. 1. Diagrammatic representation of the lower half laminectomy of lumbar vertebra: the shaded portion in red is the part to be removed to gain access to the prolapsed disc part, white shiny part in mid represents the dural covering of spinal cord

Fig. 2. Sagittal T2-weighted MRI showing L5-S1 disc prolapse
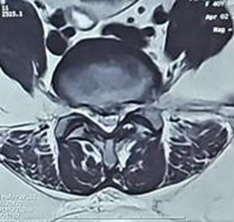
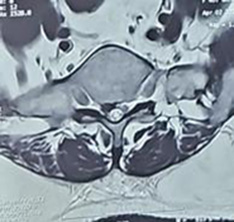
Fig. 3. Axial T2-weighted MRI showing the central disc prolapse with right-sided protusion compressing the nerve roots


Fig. 4. X-ray of the LS spine (anteroposterior (A) and lateral (B) views) done postoperatively demonstrating the post laminectomy defects(indicated by arrows)
The patients were encouraged to ambulate as soon as they could. An external orthosis (lumbar-sacral brace) was recommended for all the patients and gradually withdrawn depending on the resolutions of symptoms. The brace was typically worn longer in patients who underwent double level decompression compared to those treated at a single level.
Follow up:
Postoperative clinical assessment has been done in the next day and at discharge according to Odom’s Criteria.
Odom’s Criteria:
Results
The general characteristics and the distribution of symptoms among the population were grouped as in Table 1.
Table 1. Characteristics of the study population and distribution of symptoms
|
Characteristics |
Number of patients |
||
|
abs. |
% |
Total |
|
|
Gender distribution |
|||
|
Male |
119 |
63.3 |
188 |
|
Female |
69 |
36.6 |
|
|
Age group |
|||
|
0-20yrs |
9 |
4.8 |
188 |
|
21-40 yrs |
53 |
28.2 |
|
|
41-60 yrs |
104 |
55.3 |
|
|
>60 yrs |
23 |
12.2 |
|
|
Symptoms |
|||
|
Localized pain |
37 |
19.7 |
188 |
|
Radicular pain |
127 |
67.5 |
|
|
Sensory deficit |
93 |
49.5 |
|
|
Motor deficit |
105 |
55.8 |
|
|
Sphincter involvement |
13 |
7 |
|
|
Levels of involvement |
|||
|
L5-S1 |
81 |
43.1 |
155 |
|
L4-L5 |
57 |
30.3 |
|
|
L3-L4 |
17 |
9 |
|
|
L4-L5, L5-S1 |
21 |
11.2 |
33 |
|
L3-L4, L4-L5 |
12 |
6.4 |
|
The majority of patients were male (63.3%) with the most prevalent age group being 41-60 years (55.3%) followed by 21-40 years group (28.2%) representing the major working force of the region. Patients presented with either isolated or multiple symptoms arising out of disc proplapse varying from mono-radiculopathy or localized pain to neurological deficits(motor, sensory, autonomic). Radiculopathy was the most common symptom, observed in more than 2/3rdof the patients with a few having autonomic involvements also (7%).
Most of the surgeries (86.7%) were completed within an hour, while the rest (13.3%) were performed within the next hour. Multilevel involvement, calcified or sclerosed discs were among few reasons leading to prolonged surgical durations. Typically, the patients are discharged on the 3rd postoperative day. However, the poor patients residing in remote areas with no proper access to healthcare facilities are kept for 5-6 days, and discharged after wound inspection, unless there are complications. Postoperative complications were observed in 33 cases (17.5%) and ranged from minor surgical site infections (SSI), such as serous discharge or erythema to CSF leaks. Only 2 patients required readmissions for SSI management due tocomorbid condition (Diabetes mellitus type 2) and both were successfullydischarged the following week.The remaining cases were conservatively managed with antibiotics and other supportive measures. A subset of patients (n=25) have prolonged hospital stay of more than 7 days (Table 2).
Table 2. Distribution of various surgery-related aspects
|
|
Number of patients |
|
|
abs. |
% |
|
|
Duration of surgery |
||
|
<1 hour |
163 |
86.7 |
|
1-2 hours |
25 |
13.3 |
|
Complications |
||
|
Surgical site infection |
11 |
5.8 |
|
readmission |
2 |
1.1 |
|
Dural tear |
9 |
4.7 |
|
CSF leak |
1 |
0.05 |
|
New onset radiculopathy |
4 |
2.2 |
|
Discitis |
2 |
1.1 |
|
General complications |
7 |
3.7 |
|
Total |
33 |
17.5 |
|
Hospital Stay |
||
|
<7days |
163 |
86.7 |
|
>7days |
25 |
13.2 |
Postoperative recovery was assessed using Odom’s criteria. Majority of the patients (64% or 2/3rd) demonstrated excellent recovery at the time of discharge and this proportion gradullay improved towards each follow-up reaching 79% at 3 months. About 1/4th of patients (26%) had a good recovery while 9.6% exhibited fair recovery at the time of discharge.This number gradually progressed towards better recovery over the time with only 5% remaining in the fair category and 15% in the good category withremainder in excellent category. None of our patients had deterioration of symptoms (Table 3).
Table 3. Recovery status of patients at various intervals in post-operative period
|
Post-op recovery status |
At the time of discharge |
At first follow-up (1 month) |
At 3rd month follow up |
|||
|
abs. |
% |
abs. |
% |
abs. |
% |
|
|
Excellent |
121 |
64.3 |
143 |
76 |
149 |
79.2 |
|
Good |
49 |
26 |
33 |
17.5 |
29 |
15.4 |
|
Fair |
18 |
9.6 |
12 |
6.3 |
10 |
5.3 |
|
Poor |
- |
- |
- |
- |
- |
- |
|
Total |
188 |
|||||
Discussion
Lumbar disc pathologies are a major cause of morbidity among the Indian population, where the primary occupation of majority is agriculture and related activities. Addressing this issue, often surgical decompression is required depending on the gravity of the pathology and deficits or symptoms associated which are often not amenable to medical management. While discectomy was first initiated in 1908, since then many advancements have taken place and newer modalities like chemonucleolysis, endoscopic discectomy, microscopic discectomy, percutaneus laser-assisted decompression have come into existence. Each modality presents its own set of advantages and limitations. However,still in most parts of world andin resource-poor countries like ours, open decompression with discectomy is mostly practiced.
Various comparative studies have been done comparing the efficacy and outcomes of open discectomy with other modalities. A recent study of Pravesh et al. in 2022 comparing full endoscopic vs. open discectomy emphasized endoscopic method to bear more favorable results but differences were not clinically significant [6].Another meta-analysis, comparing endoscopic and open procedures published in 2021 concluded there were no difference in leg pain reduction or functional recovery in either groups in long term follow-up [7]. Calikoglu et al. (2018) in their study of 519 patients concluded that no significant differences in outcomes, complications and re-operations due to recurrences in either groups however significantly lesser time and hospital stays were seen in microdiscectomy groups [8]. Complication rates in post-operative periods were noted in 17.5% cases, which is comparable to previous studies by Tao et al. (16.6%) in 2018 and Xu et al. (20%) in 2020 [11, 12].
Another important outcome from this study was lesser number of anaesthetic drug usage, which also had implications for perioperative infection control.Studies pertaining to microbial contamination by injecting medications into stopcocks or I.V. ports have been done and they point out to the fact that lesser the number of drugs injected,lesser times will be the handling of IV ports and lesser will be the risk of peri-operative contaminations [9]. Other major concern with SA is hypotension. It is due to sympathetic blockade resulting to decreased venous return and preload and exacerbated by prone positioning. Vasopressors may be required . Few cases had vasopressor use intraoperatively in our study which is consistent withprevious studies. Other complications of direct nerve injury attributable to SA have been reported in previous studies, however no such complications were observed in our cohort.
Our findings are comparable to those reported in the above discussed literature [6, 10, 11, 12]. Both microdiscectomy and endoscopic discectomy present notable limitations, such as the necessity for expensive instruments, the requirement for specialized centers, and the need for advanced expertise. Moreover, these techniques are particularly ineffective in managing large central discs and ligamentum hypertrophy, as well as spinal canal pathologies beyond disc-related issues, which can lead to a heightened recurrence rate compared to open surgical approaches (Arvind et al., 2014) [10]. Although microdiscectomy and endoscopic discectomy are characterized by minimal exposure, the limited laminectomy method employed in our study provided sufficient access to the affected segment while significantly reducing the likelihood of residual disc material and delayed instability. Moreover, this technique can be executed without the need for specialized instruments, making it relatively straightforward to learn and master.
Conclusion
In a limited resource setting like ours and most parts of India, open limited laminectomy and discectomy proves to be a cost efficient method withno need of general anesthesia, early mobilization, basic instrument set requirement for spinal surgeries. The long-term outcomes are comparable to newer minimal invasive modalities and could be performed in smaller centres with basic facilities of C-arm or even portable X-ray machines. Also, the learning curve is comparatively shorter with better decompression achievable by thickened ligamentum flavum excision, when present.
Declarations
Author contribution
All the authors contributed equally to the conception of the study, development of the research design, the writing of the manuscript, research idea, and conducted the research. All authors reviewed and approved the final draft of the manuscript and take full responsibility for the content of this publication.
Ethics approval and Consent
Written informed consent was obtained from the patient/guardian. The patient’s identity has been adequately anonymized. If anything related to the patient’s identity is shown, adequate consent has been taken from the patient/relative/guardian.
Funding
No funding was received for the preparation of the manuscript
Conflict of Interest
The authors declare no conflicts of interest.
Disclosure
The authors hereby certify that the work shown here is genuine, original and has not been submitted anywhere, either in part or full.
References
1. Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK560878/2. Finneran MM, Naik A, Hawkins JC, Nardone EM. Minimally invasive bilateral decompressive lumbar laminectomy with unilateral approach: patient series. J Neurosurg Case Lessons. 2022 Feb 14;3(7):CASE21676. https://doi.org/10.3171/CASE21676
3. Zhao Z, Gu J. Open surgery in the era of minimally invasive surgery. Chin J Cancer Res. 2022 Feb 28;34(1):63-65. https://doi.org/10.21147/j.issn.1000-9604.2022.01.06
4. Estefan M, Munakomi S, Camino Willhuber GO. Laminectomy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK542274/
5. McCulloch JA. Focus issue on lumbar disc herniation: macro- and microdiscectomy. Spine (Phila Pa 1976). 1996 Dec 15;21(24 Suppl):45S-56S. https://doi.org/10.1097/00007632-199612151-00005
6. Gadjradj PS, Rubinstein SM, Peul WC, Depauw PR, Vleggeert-Lankamp CL, Seiger A, van Susante JL, de Boer MR, van Tulder MW, Harhangi BS. Full endoscopic versus open discectomy for sciatica: randomised controlled non-inferiority trial. BMJ. 2022 Feb 21;376:e065846. https://doi.org/10.1136/bmj-2021-065846
7. Gadjradj PS, Harhangi BS, Amelink J, van Susante J, Kamper S, van Tulder M, Peul WC, Vleggeert-Lankamp C, Rubinstein SM. Percutaneous Transforaminal Endoscopic Discectomy Versus Open Microdiscectomy for Lumbar Disc Herniation: A Systematic Review and Meta-analysis. Spine (Phila Pa 1976). 2021 Apr 15;46(8):538-549. https://doi.org/10.1097/BRS.0000000000003843
8. Calikoglu C, Cakir M. Open Discectomy vs. Microdiscectomy: Results from 519 Patients Operated for Lumbar Disc. Herniation. Eurasian J Med. 2018 Oct;50(3):178-181. https://doi.org/10.5152/eurasianjmed.2018.18016
9. Gargiulo DA, Mitchell SJ, Sheridan J, Short TG, Swift S, Torrie J, Webster CS, Merry AF. Microbiological Contamination of Drugs during Their Administration for Anesthesia in the Operating Room. Anesthesiology. 2016 Apr;124(4):785-94. https://doi.org/10.1097/ALN.0000000000001041
10. Kulkarni AG, Bassi A, Dhruv A. Microendoscopic lumbar discectomy: Technique and results of 188 cases. Indian J Orthop. 2014 Jan;48(1):81-7. https://doi.org/10.4103/0019-5413.125511
11. Tao XZ, Jing L, Li JH. Therapeutic effect of transforaminal endoscopic spine system in the treatment of prolapse of lumbar intervertebral disc. Eur Rev Med Pharmacol Sci. 2018 Jul;22(1 Suppl):103-110. https://doi.org/10.26355/eurrev_201807_15371
12. Xu G, Zhang C, Zhu K, Bao Z, Zhou P, Li X. Endoscopic removal of nucleus pulposus of intervertebral disc on lumbar intervertebral disc protrusion and the influence on inflammatory factors and immune function. Exp Ther Med. 2020 Jan;19(1):301-307. https://doi.org/10.3892/etm.2019.8223