Original article
Ukrainian Neurosurgical Journal. 2025;31(2):65-68
https://doi.org/ 10.25305/unj.324776
1 Department of Nervous Diseases and Neurosurgery of Faculty of Postgraduate Education, Dnipro State Medical University, Dnipro, Ukraine
2 Medical center "Endoscopic Neurosurgery", Dnipro, Ukraine
3 Department of Spinal Neurosurgery, Mechnikov Dnipropetrovsk Regional Hospital, Dnipro, Ukraine
Received: 14 March 2025
Accepted: 07 April 2025
Address for correspondence:
Mykola O. Zorin, Department of Nervous Diseases and Neurosurgery of the Faculty of Postgraduate Education, Dnipro State Medical University, 9 Volodymyr Vernadskyi Street, Dnipro, 49044, Ukraine, e-mail: nzorin@i.ua
Objective: To develop a clear treatment strategy for multilevel protrusions and herniations of the lumbar spine using the method of percutaneous laser microdiscectomy (PLMD).
Materials and Methods: The study involved 620 patients diagnosed with multilevel lumbar intervertebral disc (IVD) protrusions and herniations, all of whom underwent PLMD. The patients ranged in age from 20 to 50 years, including 360 men and 260 women. All patients underwent preoperative magnetic resonance imaging, and 62% additionally underwent computed tomography. The patients were categorized into four groups: group
I (n = 78): PLMD was performed at a single level with herniations characterized by posterior-central or paramedian localization and a sagittal size not exceeding 7 mm; group II (n = 24): PLMD was performed on discs with herniations similar to those in group I, but accompanied by protrusions at other levels (sagittal size 4–6 mm); group III (n = 380): PLMD was performed in a single session on two levels with protrusions (sagittal size 4–6 mm); group IV (n = 138): PLMD was performed in a single session on three levels with protrusions (sagittal size 4–6 mm). All procedures were performed under fluoroscopic guidance using a C-arm system (Phillips, Netherlands). Pain intensity was evaluated using the Visual Analog Scale (VAS) preoperatively and during the two-week postoperative period. Treatment outcomes after one month were assessed using the McNab scale. Long-term quality of life was evaluated using the Oswestry Disability Index.
Results: In Group I, the initial radicular pain (measured by VAS) was more severe but significantly decreased after one week postoperatively, while lumbar pain (lumbalgia) remained moderate over the two-week follow-up. In Group II, the reduction in radicular symptoms mirrored that of Group I, with the greatest treatment effect (d = 0.7, p < 0.05); however, lumbalgia only decreased after two weeks (p > 0.05). In Groups III and IV, radicular pain decreased similarly to Group II. However, in Group IV, the intensity of lumbalgia remained high and exceeded the baseline even after two weeks (p > 0.05). At the one-month follow-up, the highest rate of excellent outcomes was observed in Group I and the lowest in Group IV, though differences between the groups were not statistically significant (p > 0.05). These findings suggest that post-PLMD pain severity is largely influenced by lumbalgia rather than radicular pain.
Conclusions: Percutaneous laser microdiscectomy is an effective method for treating protrusions and non-sequestered small herniations of the lumbar spine. The method is most appropriate and efficient when performed in a single session for two symptomatic lumbar IVD protrusions. Although it is technically feasible to treat three symptomatic protrusions in a single session, such an approach is considered less advisable.
Keywords: multilevel protrusions; multilevel herniations; percutaneous laser microdiscectomy
Introduction
Protrusions and herniations of the lumbar intervertebral discs (IVDs) are among the leading causes of back pain. According to computed tomography (CT) and magnetic resonance imaging (MRI) data, disc protrusions and herniations at two or more levels are detected in approximately 50% of patients presenting with back pain [1, 2]. Although the majority of IVD protrusions are asymptomatic, there are cases in which such protrusions cause not only localized lower back pain (lumbalgia) but also radicular pain syndromes. In contrast, lumbar disc herniations are more commonly associated with radicular pain and to a lesser extent with lumbalgia. It is well established that most protrusions respond successfully to conservative treatment methods [3]. This is also true for small-sized herniations (<6 mm) without signs of sequestration. A minority of patients, however, do not benefit from conservative therapy, yet they do not meet the absolute indications for open surgical intervention. It has been found that these patients may benefit from percutaneous techniques, among which laser methods are the most widely used [4, 5]. Introduced in the 1980s, this technique has gained international traction and is now employed in many neurosurgical and orthopedic clinics [6–9]. The method has been described under various names, including nucleoplasty, intradiscal decompression, and vaporization [10, 11]. Based on the proposal by Ye.H. Pedachenko, this approach was termed "percutaneous laser microdiscectomy" (PLMD) [12]. Experimental and clinical studies have demonstrated that through the effects of ablation and vaporization, the laser beam can reduce the volume of the IVD by 15–25% [13].
Currently, there is no clear consensus regarding the management strategy for multilevel lumbar disc protrusions and herniations [14]. It remains uncertain whether multiple affected discs should be treated in a single session. If so, how many discs can be safely operated on during one procedure? Furthermore, if multiple disc interventions are permitted, what is the acceptable level of radiation exposure? These questions require definitive answers.
Objective: To develop a clear treatment strategy for multilevel protrusions and herniations of the lumbar spine using the method of percutaneous laser microdiscectomy (PLMD).
Materials and methods
The study was conducted at the “Endoscopic Neurosurgery” Medical Center (Dnipro), where PLMD procedures have been performed since 1997.
Study participants
A total of 620 patients aged between 20 and 50 years participated in the study. Among them, 360 were men and 260 were women.
All patients provided written informed consent to participate in the study.
The study protocol was approved by the ethics and bioethics committee of Dnipro State Medical University (Minutes No. 25 dated 19 February 2025).
Group characteristics
The patients were divided into four groups. Group I included 78 patients who underwent PLMD on a single IVD with posterior median or paramedian herniation, with a sagittal size not exceeding 7 mm. Group II consisted of 24 patients who underwent PLMD on a single IVD, where herniations were similar to those in group I and were accompanied by protrusions at other spinal levels (sagittal size of 4–6 mm). Group III included 380 patients who underwent PLMD in a single session on two IVDs with protrusions (sagittal size of 4–6 mm). Group IV comprised 138 patients who received PLMD in a single session on three IVDs with protrusions (sagittal size of 4–6 mm).
Inclusion criteria
Patients were selected based on criteria commonly cited in the literature [15]: age not exceeding 50 years, preservation of disc hydration and sufficient disc height (at least 2/3 of normal height), herniation size not exceeding 6 mm, absence of ossifying ligamentosis, degenerative spinal canal stenosis, and spondylolisthesis. Protrusions of at least 3 mm were considered.
Study design
Only patients treated within the last 10 years using diode lasers Surgilas (Germany) and Lika-Surgeon (Cherkasy, Ukraine) were included. The laser wavelength was 980 nm, with an energy load not exceeding 800 J per disc. The duration of each pulse was 1 second with an energy output of 15 J. All patients underwent preoperative magnetic resonance imaging (MRI) using various 1.5 Tesla machines. Additionally, 62% of the patients also had computed tomography (CT) scans performed using a 16-slice Toshiba scanner (Japan).
Surgeries were performed under fluoroscopic guidance using a C-arm system (“Philips“, Netherlands).
Pain intensity was assessed preoperatively and within 2 weeks postoperatively using the Visual Analogue Scale (VAS). Surgical efficacy was evaluated at 1 month postoperatively using the McNab classification. In the long-term follow-up, quality of life was assessed using the Oswestry Disability Index.
Statistical analysis
The analysis of the obtained data was conducted using methods of descriptive and analytical biostatistics. Quantitative indicators are presented as arithmetic mean and its standard error (M±m). The therapeutic effect size was calculated using Cohen’s d method, and its statistical significance was determined using the paired Student’s t-test. A p-value of <0.05 (<5%) was considered statistically significant for all types of analysis performed [16].
Results
The neurological status of the patients was heterogeneous. In the patients of groups I and II, radicular syndrome predominated more frequently (76.4%), while in groups III and IV, lumbalgia was more common. In groups I and II, the average severity of radicular pain syndrome was (7.3±1.6) and (7.50±1.46) points respectively, and the pain syndrome associated with lumbalgia was (6.40±0.78) and (5.30±0.91) points. In patients of groups III and IV, the respective values were (6.70±0.85) and (6.20±1.47) points, and (6.10±1.34) and (6.30±1.54) points.
In group I, laser loading was applied to the intervertebral discs from L2 to L5 with approximately 880 J, and to the L5-S1 herniated IVDs with approximately 700 J, due to the smaller volume of this disc compared to others. In this group, PLMD was limited to the herniated disc only (76.4%). In contrast, group II included PLMD of the herniated disc and, in 25.6% of cases, the additional disc with a protrusion. This was due to the presence of a predominantly radicular pain when both a hernia and one protrusion were present, prompting intervention on the herniated disc only. In patients presenting with both radicular pain and pronounced lumbalgia, PLMD was performed on both affected discs. In group III, which involved multilevel disc protrusions, the disc corresponding to the radicular pain was operated on first, followed by the disc with the more pronounced protrusion (4–6 mm). In group IV, determining the cause of lumbalgia was more complex due to the presence of three or more IVDs protrusions. In 16% of patients, the pain could be localized to a lumbar region either above or below the most affected segment. In such cases, PLMD was performed on the L1-L2, L2-L3, and L3-L4 discs or on the L3-L4, L4-L5, and L5-S1 discs. In other instances, it was not possible to determine which of the affected discs was primarily responsible for the lumbalgia. Consequently, PLMD was performed in a single session on the three IVDs with the largest protrusions.
In group I, the initial intensity of radicular pain according to the VAS was significantly higher, but it decreased within the first week and remained at a low level over the following two weeks. Meanwhile, the severity of lumbalgia remained at a moderate level during the same period (Table 1).
Table 1. Pain intensity on the VAS following percutaneous laser microdiscectomy
|
Pain type |
Group |
Number of patients |
VAS pain intensity, points |
Cohen’s d* |
||
|
Baseline |
After 1 week |
After 2 weeks |
||||
|
Radicular |
І |
78 |
7,30±1,62 |
3,60±1,44 |
2,70±0,83 |
-0,40** |
|
ІІ |
24 |
7,50±1,46 |
3,5±1,27 |
2,20±1,62 |
-0,70** |
|
|
ІІІ |
380 |
6,70±0,85 |
2,90±1,34 |
1,90±0,78 |
-0,46** |
|
|
IV |
138 |
6,20±1,47 |
2,60±1,15 |
1,80±1,52 |
-0,45** |
|
|
Lumbalgia |
І |
78 |
6,40±0,78 |
4,50±1,36 |
3,80±1,65 |
-0.22 |
|
ІІ |
24 |
5,30±0,91 |
5,90±1,83 |
4,10±1,75 |
-0,17 |
|
|
ІІІ |
380 |
6,10±1,34 |
6,20±1,46 |
4,10±0,97 |
-0,11 |
|
|
IV |
138 |
6,30±1,54 |
7,90±1,73 |
7,20±1,47 |
0,06 |
|
Notes:
* represents the effect size comparing baseline pain intensity with values after 2 weeks.
**statistically significant treatment effect (p < 0.05) according to Student’s paired t-test.
In group II, in which PLMD was performed for IVD with both herniation and protrusion, the dynamics of radicular pain were similar to those observed in group I. The treatment effect on radicular pain was the most pronounced in this group (d = 0.7, p < 0.05). At the same time, the intensity of lumbalgia during the first week even increased and only began to slightly decrease after two weeks; however, this effect was not statistically significant (p > 0.05).
The dynamics of pain syndrome in patients of groups III and IV did not differ significantly from group II regarding radicular pain: a gradual decrease in pain intensity was observed within the first week and continued in the second week. However, in patients of group IV, who underwent PLMD in a single session for three IVDs with protrusions, the intensity of lumbalgia was significantly higher than in the other groups. After two weeks, this value remained higher than at baseline (p > 0.05), indicating a more severe post-procedural response in these patients.
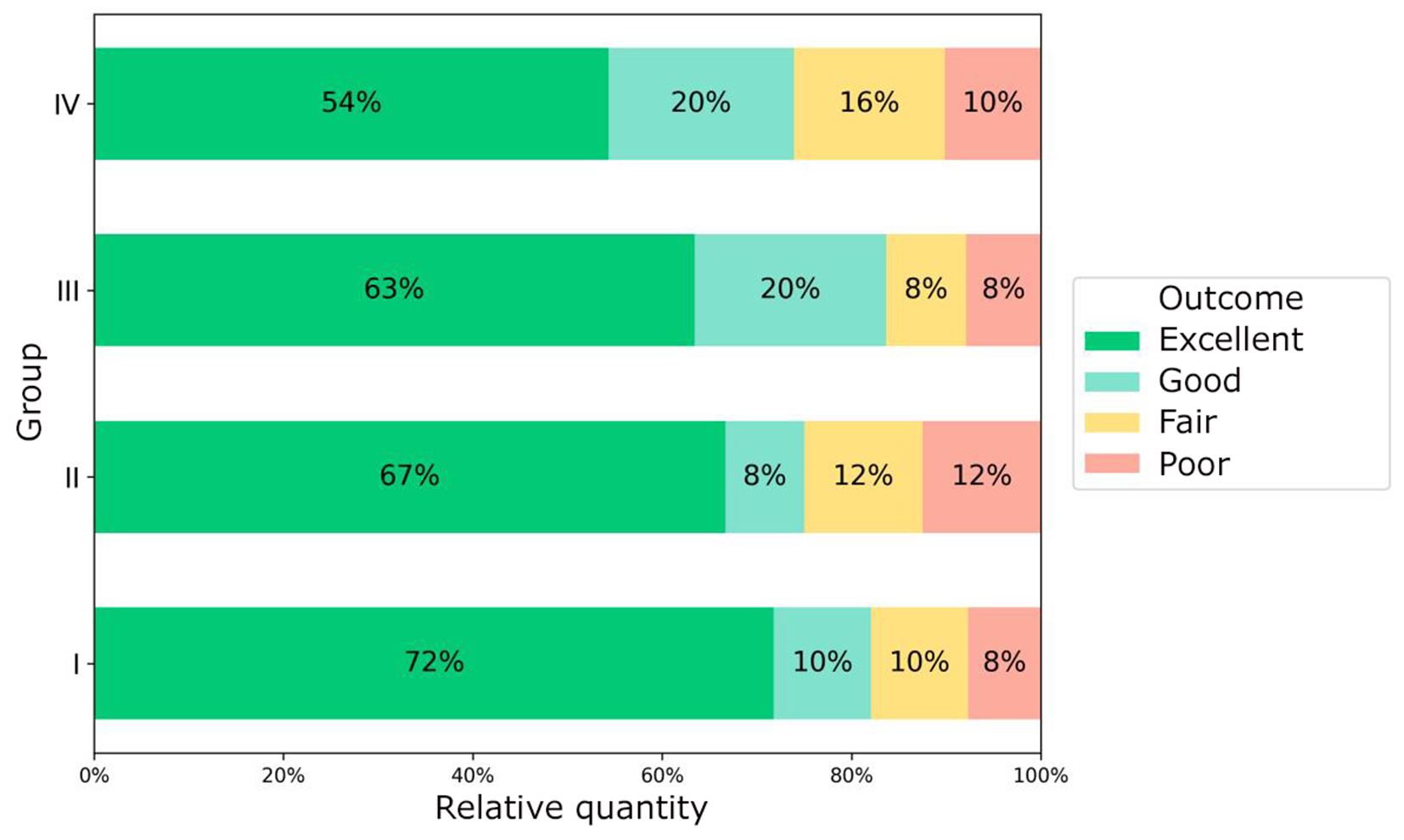
One month after PLMD, the patients' condition was assessed using the McNab scale (Fig. 1). The highest frequency of excellent outcomes was recorded in Group I, while the lowest was observed in Group IV; however, the differences between the groups were not statistically significant (p>0.05). It can be assumed that the intensity of pain following PLMD is largely associated with lumbalgia rather than radicular pain. At the same time, a tendency was observed: as the number of IVDs treated with PLMD during a single session increased, patients experienced greater difficulty tolerating lumbalgia.
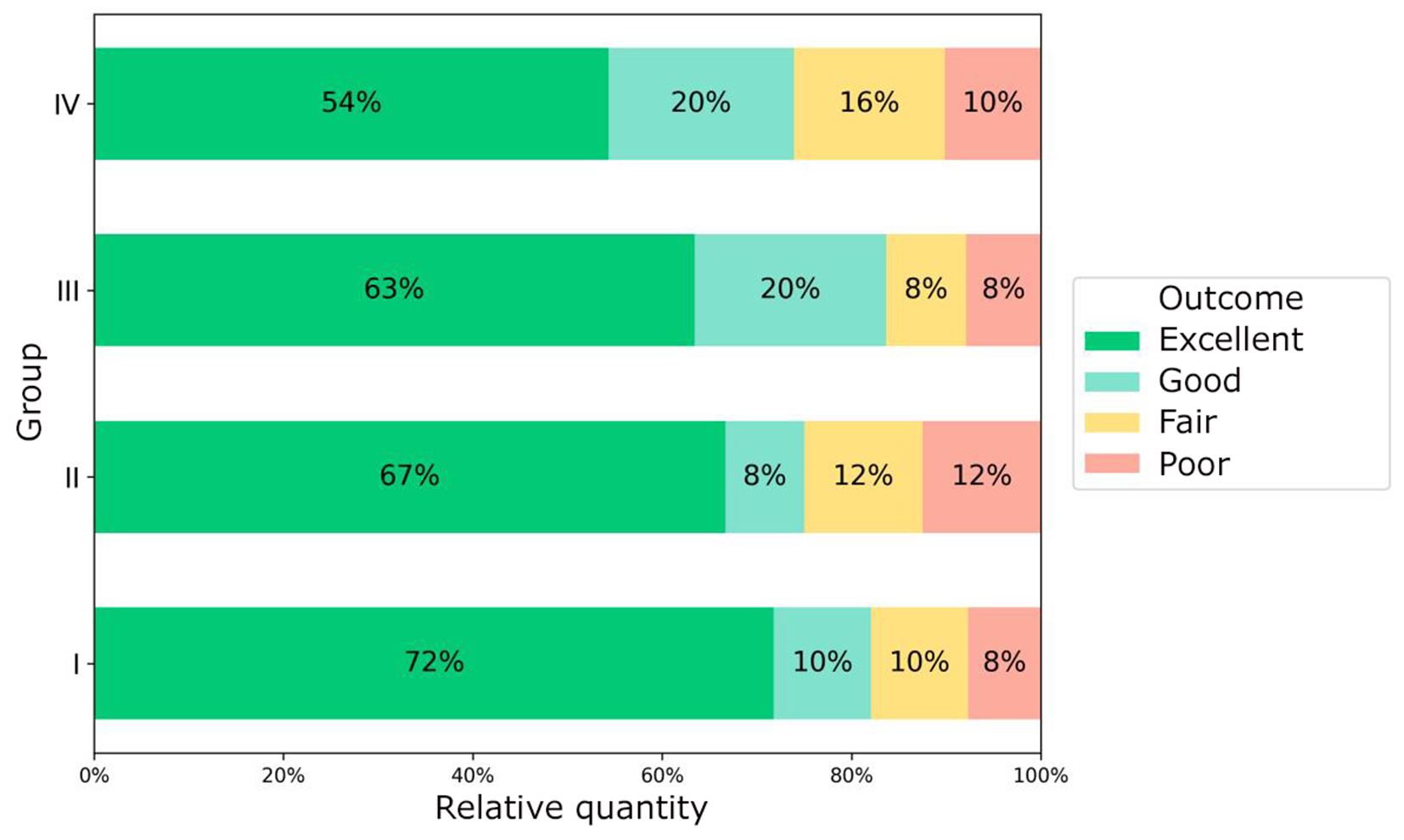
Fig. 1. Assessment of patients’ condition after percutaneous laser microdiscectomy using the McNab scale
Long-term outcomes were evaluated using the Oswestry Disability Index before surgery and at various intervals thereafter. A total of 312 patients were successfully followed up and provided responses. The average follow-up duration was (2.40 ± 0.38) years.
The outcomes obtained using the Oswestry Disability Index (Table 2) indicated that in all groups, a statistically significant improvement was observed in the long-term follow-up period (p<0.001 for each group separately). The largest effect sizes were recorded in group II (d = ‒2.02, p<0.001) and group I (d = ‒1.18, p<0.001). These findings suggest that PLMD is an effective treatment for lumbar disc protrusions and small herniations of the lumbar spine. Procedures performed on two levels in a single session resulted in a slight deterioration in patients' conditions during the first two weeks postoperatively, particularly in group IV. However, one month after surgery, a significant clinical improvement was observed across all patient groups. According to the McNab criteria, patients who underwent PLMD on three levels in one session showed poorer early outcomes. Nevertheless, in the long-term follow-up, the results across all groups were comparable. This supports the conclusion that performing PLMD on two lumbar IVDs in one session is sufficiently effective. Patients in this category experienced mild deterioration in the early postoperative period, which was generally well tolerated, and by one month post-surgery, their condition was similar to that of group I, where PLMD was performed on a single IVD. In contrast, patients in group IV experienced an intensified pain syndrome of the lumbalgia type in the early postoperative period, which significantly worsened their overall condition. Although their condition improved one month after surgery, it did not reach the levels observed in the other groups. In the long-term follow-up, the quality of life of patients in group IV, as measured by the Oswestry Disability Index, remained worse than in the other groups. This suggests that performing PLMD on three IVDs in a single session increases radiation load on the lumbar spine, which negatively affects patient outcomes. Therefore, in our opinion, while technically feasible, PLMD on three IVDs in one session is not advisable.
Table 2. Evaluation of quality of life in the long-term period after percutaneous laser microdiscectomy using the Oswestry Disability Questionnaire
|
Group |
Number of patient responses |
Before surgery, % |
In the long-term period, % |
Cohen’s d |
p |
|
І |
46 |
78,3±6,72 |
21,5±7,45 |
-1,18 |
<0,001 |
|
ІІ |
20 |
79,8±7,22 |
20,3±5,87 |
-2,02 |
<0,001 |
|
ІІІ |
167 |
75,8±6,89 |
18,6±6,64 |
-0,65 |
<0,001 |
|
IV |
79 |
73,7±5,97 |
27,7±7,87 |
-0,74 |
<0,001 |
Conclusions
Disclosure
Conflict of interest
The authors declare no conflict of interest.
Ethical standards
All procedures involving patients during the study complied with the ethical standards of institutional and national ethics committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
The study received no external funding or sponsorship.
References
1. He S, Sun Z, Wang Y, Ma D, Tan W, Lai J. Combining YESS and TESSYS techniques during percutaneous transforaminal endoscopic discectomy for multilevel lumbar disc herniation. Medicine (Baltimore). 2018 Jul;97(28):e11240. https://doi.org/10.1097/MD.0000000000011240
2. Zorin MO, Ovcharenko DV, Shulga OM, Zorin MM. Surgical tactics for multilevel displacements of lumbar intervertebral discs. Ukrainian Neurosurgical Journal. 2019;25(4):57-63. https://doi.org/10.25305/unj.182500
3. Gugliotta M, da Costa BR, Dabis E, Theiler R, Jüni P, Reichenbach S, Landolt H, Hasler P. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open. 2016 Dec 21;6(12):e012938. https://doi.org/10.1136/bmjopen-2016-012938
4. Hashemi M, Falsafi M, Razzaghi MR, Dadkhah P, Taheri M, Delshad MH, Zali A. The Long-term Effects of Percutaneous Laser Disc Decompression (PLDD) Treatment on Lumbar Disc Protrusion: A 2-Year Follow-up. J Lasers Med Sci. 2020 Fall;11(4):427-432. https://doi.org/10.34172/jlms.2020.67
5. Erbas YC, Pusat S, Erdogan E. Percutaneous Laser Disc Decompression: Retrospective Analysis of 197 Cases and Review of The Literature. Turk Neurosurg. 2015;25(5):766-70. https://doi.org/10.5137/1019-5149.JTN.14692-15.2
6. Momenzadeh S, Koosha A, Kazempoor Monfared M, Bairami J, Zali A, Ommi D, Hosseini B, Hashemi M, Sayadi S, Aryani R, Nematollahi F, Nematollahi L, Barati M. The Effect of Percutaneous Laser Disc Decompression on Reducing Pain and Disability in Patients With Lumbar Disc Herniation. J Lasers Med Sci. 2019 Winter;10(1):29-32. https://doi.org/10.15171/jlms.2019.04
7. Choy DS. Percutaneous laser disc decompression: a 17-year experience. Photomed Laser Surg. 2004 Oct;22(5):407-10. https://doi.org/10.1089/pho.2004.22.407
8. Brouwer PA, Brand R, van den Akker-van Marle ME, Jacobs WC, Schenk B, van den Berg-Huijsmans AA, Koes BW, Arts MA, van Buchem MA, Peul WC. Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: Two-year results of a randomised controlled trial. Interv Neuroradiol. 2017 Jun;23(3):313-324. https://doi.org/10.1177/1591019917699981
9. Hellinger J, Stern S, Hellinger S. Nonendoscopic Nd-YAG 1064 nm PLDN in the treatment of thoracic discogenic pain syndromes. J Clin Laser Med Surg. 2003 Apr;21(2):61-6. https://doi.org/10.1089/104454703765035475
10. Budrovac D, Radoš I, Tot OK, Haršanji Drenjančević I, Omrčen I. Percutaneous Laser Disc Decompression in the Treatment of Lumbar Radicular Pain. Southeastern European Medical Journal: SEEMEDJ. 2020 Nov 12;4(2):62-8.
11. Gelalis I, Gkiatas I, Spiliotis A, Papadopoulos D, Pakos E, Vekris M, Korompilias A. Current Concepts in Intradiscal Percutaneous Minimally Invasive Procedures for Chronic Low Back Pain. Asian J Neurosurg. 2019 Jul-Sep;14(3):657-669. https://doi.org/10.4103/ajns.AJNS_119_17
12. Pedachenko EG, ed. [Diagnosis and surgical treatment of discogenic neurocompression syndromes of the spine]. Kyiv: VIK-PRINT, 2014. Ukrainian.
13. Zorin MO, Zorina TV, Zorin MM. Puncture laser micro-diskectomy: 20-year experience. Ukrainian Neurosurgical Journal. 2018;(1):60-5. https://doi.org/10.25305/unj.117768
14. Malik K. Treatment of multilevel degenerative disc disease with intradiscal electrothermal therapy. Anaesth Intensive Care. 2007 Apr;35(2):289-93. https://doi.org/10.1177/0310057X0703500223
15. Maksymowicz W, Barczewska M, Sobieraj A. Percutaneous laser lumbar disc decompression - mechanism of action, indications and contraindications. Ortop Traumatol Rehabil. 2004 Jun 30;6(3):314-8.
16. Lang TA, Secic M. How to report statistics in medicine: annotated guidelines for authors, editors, and reviewers. ACP Press; 2006.