
Original article
Ukrainian Neurosurgical Journal. 2025;31(2):55-64
https://doi.org/10.25305/unj.322446
Department of Neurosurgery, Kharkiv National Medical University, Kharkiv, Ukraine
Received, 07 February 2025
Accepted, 03 April 2025
Address for correspondence:
Artem V. Stogniy, Department of Neurosurgery, Kharkiv National Medical University, 4 Nauka Prospect, Kharkiv, 61000, Ukraine, e-mail: astognii@gmail.com
Objective to improve the effectiveness of treatment of patients with lumbar spondylolisthesis, the authors substantiated and developed a novel method of minimally invasive posterior interbody vertebral stabilization (MIPIVS) using distraction cages.
Materials and methods: A clinical prospective comparative (controlled) single-center interventional cross-section study was conducted with a subsequent observation phase, as well as preliminary modeling and development of a noveltervention method. The biomechanical model was used to determine the possibility of restoring the functional state of the spine using distraction cages, and the stress-strain state of the structures was analyzed. The clinical part of the study involved 21 patients aged 35 to 68 (Me=56 [LQ=50; UQ=65]) years (15 women and 6 men), divided into three groups: the study group (n=4) treated with the author's method of MIPIVS (patent application No. a202302383 dated May 18, 2023), a comparison group (n=10) with the standard method of MIPIVS, a control group (n=7) treated with other methods of interbody spondylodesis. Patients were examined according to standard protocols. Logistic and statistical analyses were performed using standard nonparametric methods at a critical level of p<0.05. The principles of bioethics and biomedicine were observed.
Results: Before and after surgical treatment of patients with degenerative spondylolisthesis of the lumbar spine, the size of the spinal canal was studied and the dynamics of neurological disorders was assessed. The authors developed a novel method of minimally invasive posterior interbody stabilization of vertebrae using distraction cages and determined the possibility of restoring the value of segmental lordosis, parameters of spinal-pelvic balance and sagittal contour of the spine as indicators of the functional state of the spine using a biomechanical model. The analysis also included assessment of the stress-strain state within the "transpedicular structure – spinal motion segment – distraction cage" system.
Сonclusions: The proprietary method of MIPIVS using distraction cages, which has been substantiated and developed, will help to improve the effectiveness of treatment for patients with lumbar spondylolisthesis. Further research prospects include clinical testing of the author's MIPIVS method.
Key words: spondylolisthesis; treatment; operation; surgery; minimally invasive posterior interbody stabilization of the spine
Lumbar spondylolisthesis (LS) remains a significant issue in spinal surgery [1–5]. In cases where conservative treatment failed, surgical intervention was typically employed. However, the development of minimally invasive techniques has improved patient management with LS by reducing hospital stays and enhancing rehabilitation outcomes [6–10].
The application of minimally invasive posterior interbody vertebral stabilization (MIPIVS), either as a standalone procedure or using distraction cages, represents a promising approach that aligns with current trends toward preserving normal anatomy and minimizing surgical trauma [11].
The necessity for implementing and refining minimally invasive approaches is driven by numerous global geopolitical crises. The war in Ukraine poses not only a challenge to the national healthcare system but is also associated with a rising incidence of traumatic spinal injuries and multiple post-traumatic and degenerative disorders, including spondylolisthesis [12, 13].
The impact of war extends to healthcare logistics, leading to limited access to medical devices and the need for especially meticulous provisioning during surgical procedures. Preference is given to techniques that achieve the desired clinical outcomes with shorter operation times and lower resource consumption compared to extensive surgical interventions. In this context, the justification and development of effective minimally invasive surgical techniques—such as MIPIVS with distraction cages (Fig. 1)—constitute a highly relevant objective.

Fig. 1. The Designed distraction cage
Numerous medical centers are developing and implementing minimally invasive methods of interbody (particularly posterior) vertebral stabilization in cases of LS [14]. Traditional and minimally invasive posterior approaches are commonly used due to their acceptable fusion rates and low complication levels. However, these approaches are limited by the extent of dural and spinal nerve root retraction, and they carry the risk of iatrogenic injury to the paravertebral muscles and disruption of the posterior ligamentous complex. Anterior approaches, which allow bypassing the spinal canal, cauda equina, and spinal nerve roots, are associated with abdominal and vascular complications, while lateral approaches carry a risk of injury to the lumbar plexus and gluteal muscle [15].
Therefore, improving the surgical treatment of spondylolisthesis, particularly through the use of MIPIVS, remains a relevant clinical challenge.
Objective: To enhance the effectiveness of treatment for patients with lumbar spondylolisthesis by employing minimally invasive posterior interbody vertebral stabilization using distraction cages.
Materials and methods
Study design
A clinical, prospective, comparative (controlled), single-center cross-sectional interventional study was conducted (Fig. 2).
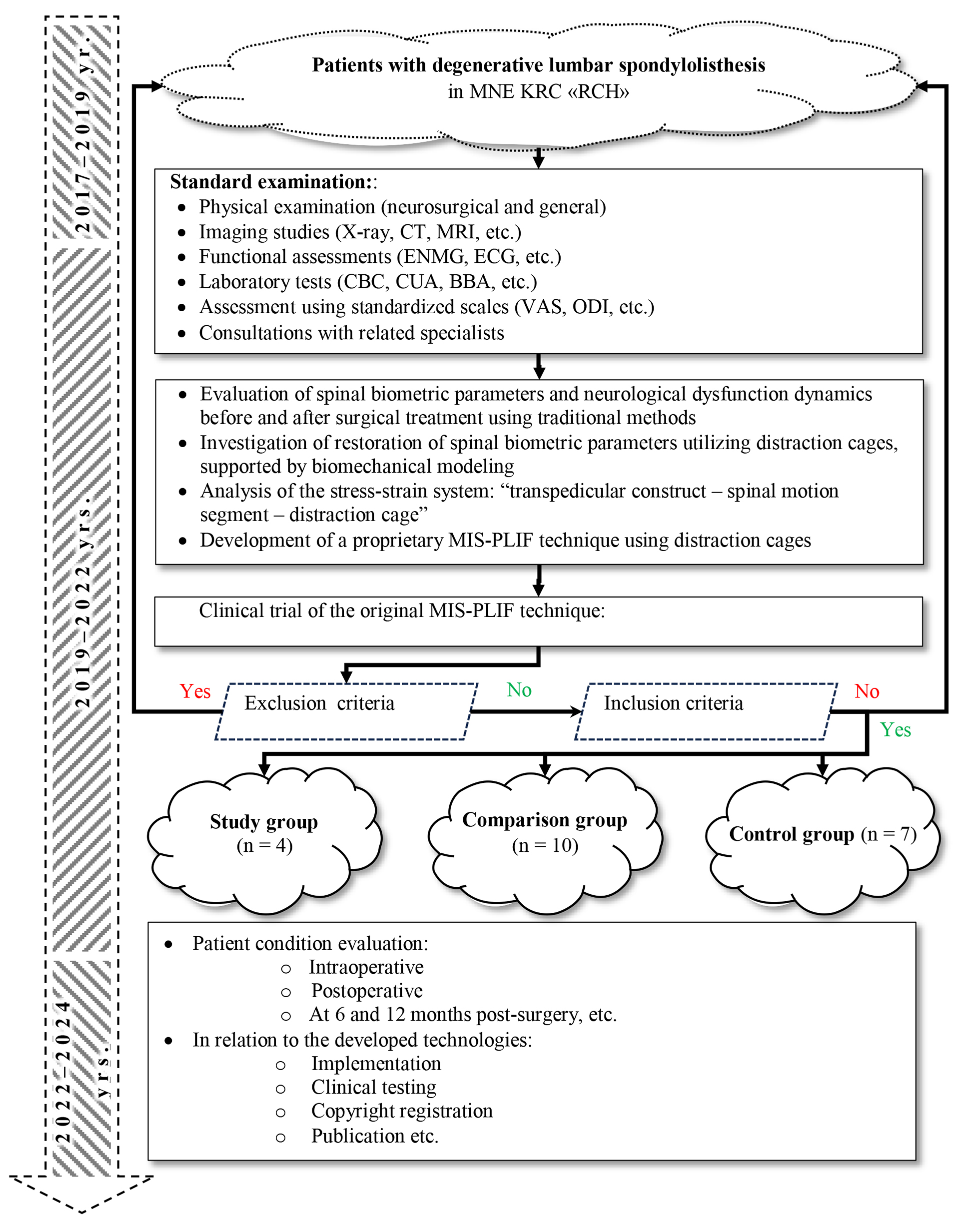
Fig. 2. Study Design:
MNE KRC «RCH»– Municipal Non-Commercial Enterprise of the Kharkiv Regional Council "Regional Clinical Hospital"; CT – computed tomography (X-ray); MRI – magnetic resonance imaging;
ENMG – electroneuromyography; ECG – electrocardiography; CBC – complete blood count; CUA – clinical urinalysis; BBA – biochemical blood analysis; VAS – visual analogue scale;ODI – Oswestry Disability Index; MIS-PLIF – minimally invasive surgery posterior lumbar interbody fusion.
Using a biomechanical model with distraction cages, the study assessed the potential for restoring segmental lordosis, spinal-pelvic balance parameters, and sagittal spinal alignment as indicators of spinal functional status. It also analyzed the stress-strain condition within the system "transpedicular construct – spinal motion segment – distraction cage" [16] in the Biomechanics Laboratory of the Sytenko Institute of Spine and Joint Pathology, National Academy of Medical Sciences of Ukraine.
The clinical study included patients with degenerative spondylolisthesis of the lumbar spine and neurocompressive disorders who underwent inpatient treatment in Neurosurgery Department No. 2 between 2017 and 2024, followed by dynamic outpatient monitoring at the clinic of the Municipal Non-Commercial Enterprise of the Kharkiv Regional Council "Regional Clinical Hospital" (Kharkiv).
The research was conducted at the Department of Neurosurgery of Kharkiv National Medical University.
The study complied with the principles of bioethics and biomedicine (ethics and bioethics committee Minutes No. 7 of Kharkiv National Medical University, dated October 10, 2017).
Study Participants
The clinical study involved 21 patients (15 women and 6 men), aged 32 to 68 years (median age – 56 (50; 65) years), divided into three groups: study group (n=4), where the author's technique of MIPIVS was applied (patent application No. a202302383 of 18.05.2023) (Fig. 3); comparison group (n=10), where the standard MIPIVS technique was used (Fig. 4); control group (n=7), where other interbody fusion techniques were employed (Fig. 5) .
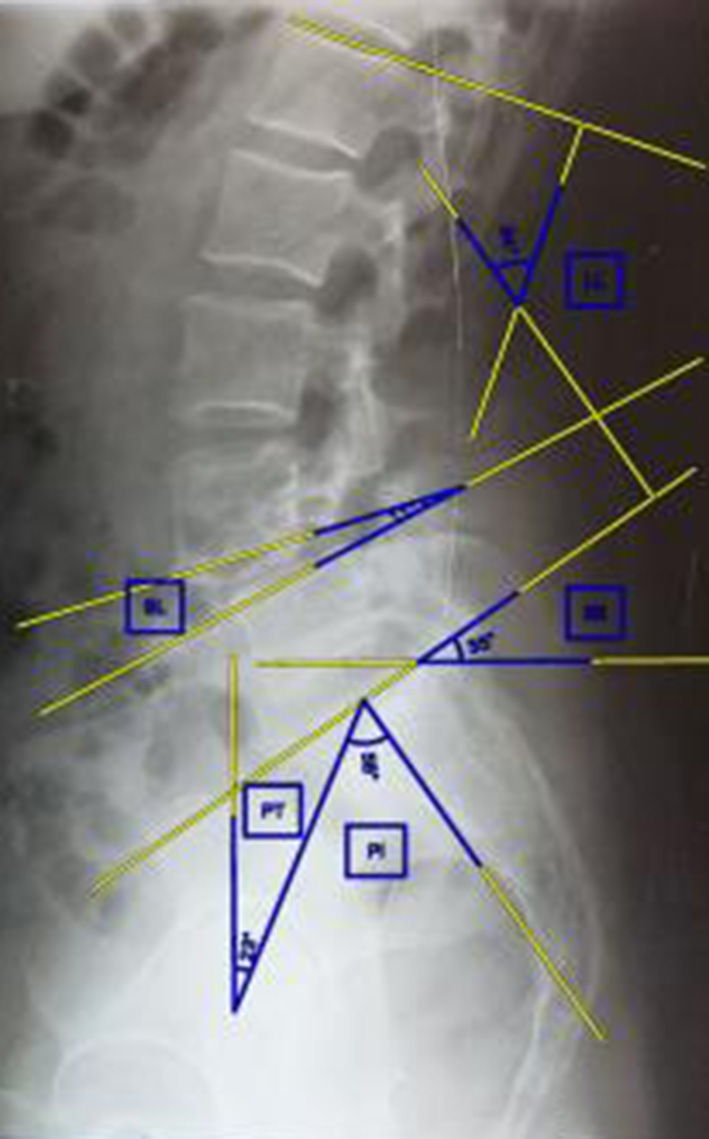
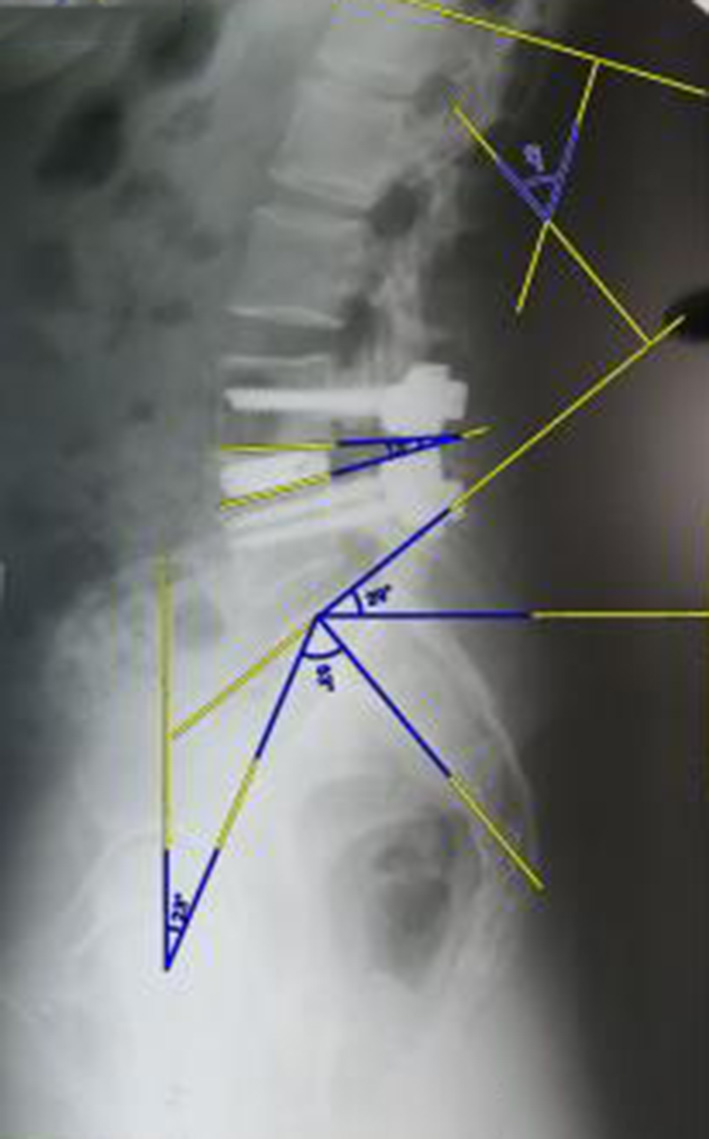
Fig. 3. Radiographic control before and after surgery using the minimally invasive posterior interbody vertebral stabilization technique with titanium distraction cages
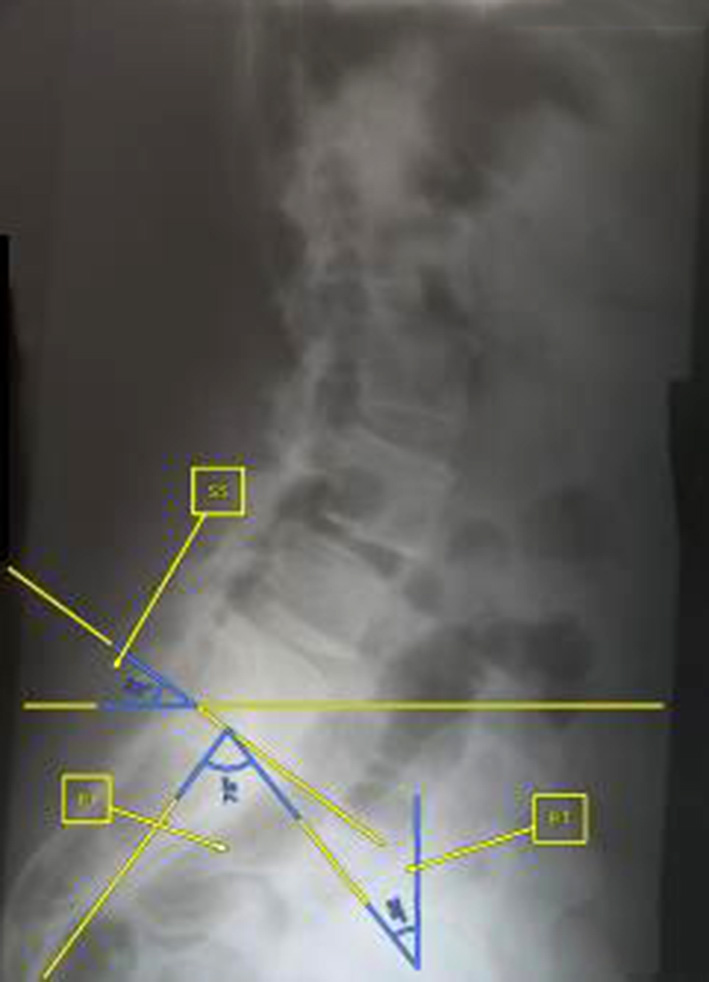
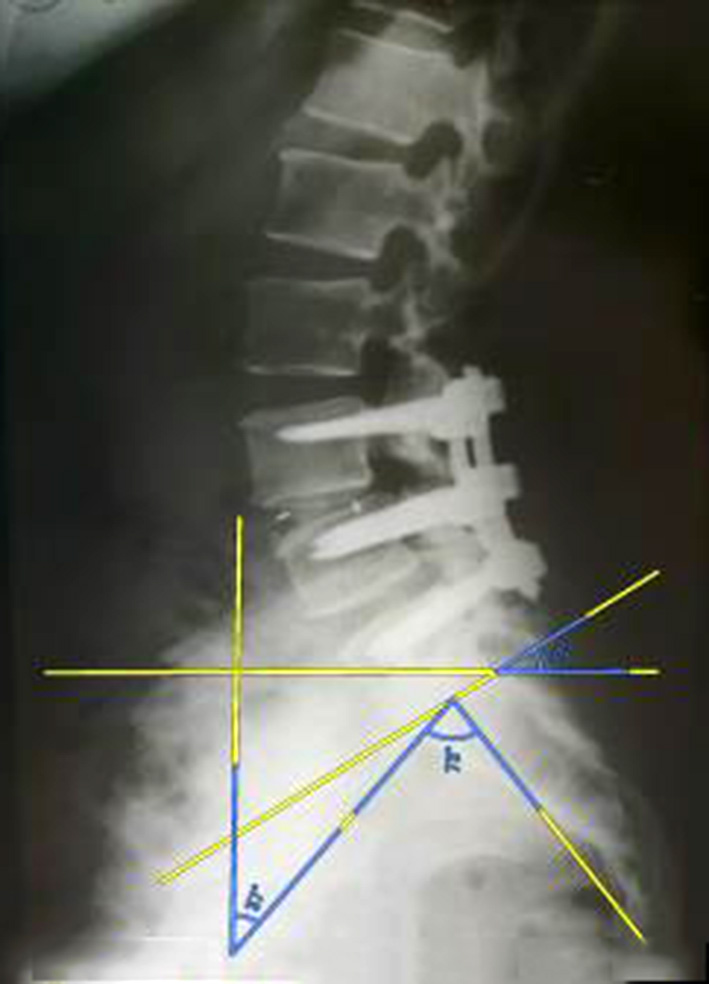
Fig. 4. Radiographic control before and after surgery using the traditional minimally invasive posterior interbody vertebral stabilization (MIPIVS) technique

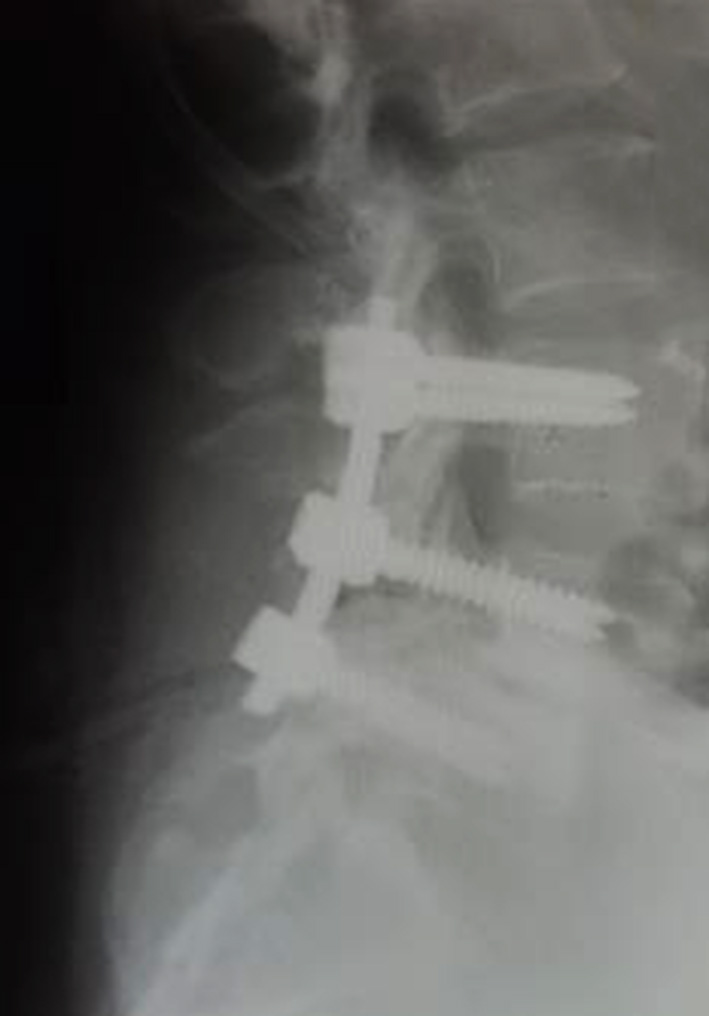
Fig. 5. Radiographic control before and after surgery using alternative methods of lumbar interbody spinal fusion
Inclusion Criteria:
diagnosed degenerative spondylolisthesis of the lumbar spine accompanied by neurocompressive disorders such as neurogenic intermittent claudication, lower limb paresis (3–4 points), and segmental sensory disturbances (L4–L5, L5–S1);
age range: 32–68 years;
surgical treatment:
- for the study group: the proposed MIPIVS technique using titanium distraction cages;
- for the comparison group: traditional MIPIVS technique;
- for the control group: alternative methods of lumbar interbody spinal fusion.
Exclusion Criteria:
Age over 75 years;
absence of neurological symptoms or neurocompressive disorders such as lower limb paresis (1–2 points) or limb plegia;
severe somatic and concomitant neurological pathology, vascular disorders of the lower extremities, etc.;
patient refusal to participate in the study.
Patients were examined according to standard protocols. The type and stage of spondylolisthesis were determined, as well as the degree of sagittal imbalance and associated neurocompressive and biomechanical disorders. This allowed for the calculation of the required intraoperative correction of lordosis to achieve optimal biomechanical compensation, etc.
Following preoperative preparation, minimally invasive surgery was performed using a standard technique with the application of an interbody distraction cage. On the first postoperative day, in the absence of contraindications, patients underwent follow-up radiographic examination to evaluate the extent of correction and calculate key biomechanical parameters (lordosis angle, sacral slope, pelvic tilt variability, and pelvic incidence relative to the sagittal vertical axis).
A neurological assessment was conducted to evaluate postoperative changes in neurological status, pain intensity using the Visual Analogue Scale (VAS), and functional status based on the Oswestry Disability Index (ODI).
On postoperative day 30, in the absence of contraindications, follow-up magnetic resonance imaging (MRI) was performed to assess the formation of primary bone fusion, along with a clinical and neurological examination, pain assessment via VAS, and functional status evaluation using the ODI.
Statistical Analysis
Data systematization and logical-statistical analysis were carried out using standard methods with a critical significance level of p<0.05. Since the data distribution deviated from normal, nonparametric statistical methods were applied. The central tendency was described using the median (Me), and variability was expressed through the determination of the lower (LQ) and upper (UQ) quartiles. The significance of pairwise intergroup differences was assessed using the Mann–Whitney U test. Frequency indicators (both absolute and relative) were compared using Fisher’s exact test.
Results and discussion
Among the clinically significant parameters, the key outcome indicators were evaluated, including complaints and medical history, physical examination data (general condition, level of consciousness), duration of the surgery, surgical approach, closure of the surgical wound, intraoperative radiation exposure to medical personnel and patients, volume of intraoperative blood loss and hemotransfusion, postoperative drainage, length of hospital stay, and the incidence of complications (radiculitis, radicular dysfunction, foot flexor weakness, pain during flexion and extension of the foot, paresthesia, motor disorders, incomplete spinal fusion, pseudoarthrosis, dural tears, major vascular injuries, neural structure damage, surgical site infection, paravertebral muscle atrophy, postoperative bleeding, cerebrospinal fluid leakage, venous thromboembolism), screw loosening, malposition of surgical hardware, reoperation, body mass index, lordosis angle, lifestyle, progression of disorders, duration of conservative treatment, pain reduction after surgery, percentage of displacement before and after surgery, increase in intervertebral space, height of the foraminal opening, disability according to the ODI, and others.
The study groups were comparable in terms of age, gender ratio, anthropometric, clinical-anamnestic, and physical characteristics (p>0.05) (Table 1).
Table 1. Clinical and anthropometric characteristics of patients with lumbar spine spondylolisthesis
|
Parameter |
Study group |
Comparison group |
Control group |
Total |
|
Age, years |
50 [37;53] |
63 [50;66] |
59 [53;60] |
50 [37;53] |
|
Men |
1 (25%) |
4 (40%) |
1 (14%) |
6 (29%) |
|
Women |
3 (75%) |
6 (60%) |
6 (86%) |
15 (71%) |
|
Body mass index, kg/m2 |
32 [28;34] |
32 [28;34] |
32 [28;34] |
32 [28;34] |
|
General condition |
RS |
RS |
RS |
RS |
|
Conciousness |
Clear |
Clear |
Clear |
Clear |
|
Achilles reflex |
Weakend |
Weakend |
Weakend |
Weakend |
|
Tenderness |
Present |
Present |
Present |
Present |
|
Lasègue sign |
Positive |
Positive |
Positive |
Positive |
|
Wassermann sign |
Positive |
Positive |
Positive |
Positive |
|
Hypoesthesia |
Present |
Present |
Present |
Present |
|
Hyperesthesia |
Present |
Present |
Present |
Present |
|
Meningeal signs |
Absent |
Absent |
Absent |
Absent |
|
Plantar signs |
Absent |
Absent |
Absent |
Absent |
|
Coordination |
Preserved |
Preserved |
Preserved |
Preserved |
|
Paresis |
Present |
Present |
Present |
Present |
Note: RS – relatively satisfactory.
The surgical parameters were more favorable in the main group (Table 2).
Table 2. Surgical parameters for lumbar spine spondylolisthesis surgery
|
Parameter |
Study group |
Comparison group |
Control group |
Total |
|
Hospital length of stay, days |
13 [11;18] |
9 [7;12] |
11 [6;22] |
10 [7;15] |
|
Duration of surgery, minutes |
180 [180;180] # |
180 [160;210] |
360 [240;480] |
180 [180;215] |
|
Duration of surgical approach, minutes |
30 [30;30] *# |
60 [60;60] |
60 [60;90] |
60 [30;60] |
|
Duration of surgical wound closure, minutes |
10 [8;10] *# |
40 [40;40] |
45 [40;50] |
40 [12;40] |
|
Duration of intraoperative radiation exposure of medical personnel, seconds |
92 [87;93] |
93 [90;95] |
87 [81;90] |
91 [87;94] |
|
Total intraoperative radiation exposure of medical personnel, mSv: |
0,22 [0,19;0,23] |
0,25 [0,21;2,18] |
0,20 [0,08;0,26] |
0,23 [0,20;0,48] |
|
Surgeon at the patient’s side, mSv |
0,08 [0,07;0,08] |
0,09 [0,07;1,05] |
0,07 [0,03;0,09] |
0,08 [0,07;0,18] |
|
Assisting staff at medium distance, mSv |
0,06 [0,05;0,07] |
0,07 [0,07;0,09] |
0,06 [0,02;0,08] |
0,07 [0,06;0,08] |
|
Other personnel at a greater distance, mSv |
0,03 [0,03;0,04] |
0,05 [0,04;0,08] |
0,04 [0,01;0,05] |
0,23 [0,20;0,48] |
|
Intraoperative patient exposure, mSv |
2 [1;4] |
1 [1;2] |
1 [1;5] |
2 [1;3] |
|
Intraoperative blood loss, ml |
100 [100;100] *# |
200 [200;300] |
500 [400;600] |
200 [100;400] |
|
Haemotransfusion |
Not performed |
1 (10%) |
Not performed |
1 (5%) |
|
Haemotransfusionvolume, ml |
‒ |
600 [600;600] |
‒ |
600 [600;600] |
|
Postoperative drainage |
Not performed |
3 (30%) |
1 (14%) |
4 (19%) |
|
Postoperative drainage volume, ml |
‒ |
0 [0;300] |
0 [0;300] |
0 [0;0] |
|
Pain reduction after surgery, difference score |
4 [4;4]# |
3 [3;4] |
2 [1;2] |
3 [3;4] |
|
Displacement, %: |
||||
|
preoperatively |
20 [20;25] |
17,5 [10;30] |
25 [20;30] |
20 [15;30] |
|
postoperatively |
5 [5;5] |
5 [0;15] |
15 [0;25] |
5 [0;15] |
|
Sagittal vertical axis displacement, cm: |
||||
|
preoperatively |
10 [8;11] |
10 [7;12] |
10 [8;12] |
10 [8;12] |
|
postoperatively |
5 [4;6] |
6 [5;7] |
6 [5;8] |
6 [5;7] |
|
Pelvic tilt angle, deg: |
||||
|
preoperatively |
50 [49;52] |
50 [48;53] |
58 [56;60] |
54 [50;57] |
|
postoperatively |
52 [51;53] |
52 [50;55] |
60 [58;62] |
56 [54;58] |
|
Pelvic incidence angle, deg: |
||||
|
preoperatively |
19 [18;20] |
24 [22;27] |
30 [29;33] |
25 [23;27] |
|
postoperatively |
16 [15;17] |
22 [20;25] |
28 [26;30] |
25 [19;23] |
|
Sacral slope angle, deg: |
||||
|
preoperatively |
31 [30;32] |
30 [28;33] |
30 [28;32] |
31 [30;32] |
|
postoperatively |
34 [33;35] |
32 [30;35] |
33 [31;35] |
33 [31;35] |
|
Increase in intervertebral space, mm |
10 [9;11] * |
8 [5;9] |
11 [8;12] |
9 [7;10] |
|
Increase in foraminal height, mm |
2,1 [2,0;2,1 ] |
2,2 [1,9;2,2] |
1,9 [1,8;1,9] |
2,1 [1,9;2,2] |
|
Duration of conservative treatment, months |
12 [12;12] |
12 [3;18 ] |
12 [12;18] |
12 [6;18] |
|
Duration of rehabilitation, months |
6 [6;6] |
6 [6;12] |
12 [6;18] |
6 [6;12] |
|
Dynamics of ODI disability, score |
10 [10;15] |
15 [10;25] |
18 [10;20] |
15 [10;20] |
Note: * – statistically significant difference from the comparison group (p<0.05); # ‒ the difference from the control group is statistically significant (p<0.05).
The incidence of complications was the lowest in the study group (Table 3). No cases of postoperative hemorrhage, cerebrospinal fluid leakage, venous thromboembolism, paravertebral muscle atrophy, incomplete spondylodesis, dural injury, screw loosening, malposition of surgical hardware, neural structure damage, major vascular injury, or surgical site infection were recorded in this group. Only one reoperation was performed due to pseudoarthrosis.
Table 3. Incidence of complications following surgical intervention for lumbar spine spondylolisthesis
|
Parameter |
Study group |
Comparison group |
Control group |
Total |
|
Postoperative hemorrhage |
‒ |
3 (30%) |
1 (14%) |
4 (21%) |
|
Postoperative cerebrospinal fluid (CSF) leakage |
‒ |
1 (10%) |
‒ |
1 (5%) |
|
Venous thromboembolism |
‒ |
‒ |
‒ |
‒ |
|
Atrophy of the paravertebral muscles |
‒ |
10 (100%) |
1 (14%) |
11 (52%) |
|
Radiculitis with dysfunction of spinal nerve roots, manifested as: |
1 (25%) |
3 (30%) |
1 (14%) |
5 (24%) |
|
Autonomic disturbances: |
||||
|
Frequency |
4 (100%) |
10 (100%) |
2 (29%) |
16 (76%) |
|
Duration (weeks) |
1 |
1 |
1 |
1 |
|
Hypoesthesia: |
|
|
|
|
|
Frequency |
1 (25%) |
4 (40%) |
1 (14%) |
6 (29%) |
|
Duration (weeks) |
1 |
1 |
1 |
1 |
|
Pain during foot flexion and extension: |
||||
|
Frequency |
1 (25%) |
3 (30%) |
1 (14%) |
5 (24%) |
|
Duration (weeks) |
1 |
1 |
1 |
1 |
|
Paresthesia: |
||||
|
Frequency |
4 (100%) |
3 (30%) |
1 (14%) |
8 (38%) |
|
Duration (weeks) |
1 |
2 |
2 |
2 |
|
Weakness of foot flexors: |
||||
|
Frequency |
‒ |
2 (20%) |
1 (14%) |
3 (14%) |
|
Duration (weeks) |
‒ |
4 |
4 |
4 |
|
Screw loosening |
‒ |
1 (10%) |
1 (14%) |
2 (10%) |
|
Malposition of surgical hardware |
‒ |
1 (10%) |
1 (14%) |
2 (10%) |
|
Incomplete spinal fusion (insufficient spondylodesis) |
‒ |
1 (10%) |
1 (14%) |
2 (10%) |
|
Dural sac injury |
‒ |
2 (20%) |
‒ |
2 (10%) |
|
Damage to neural structures |
‒ |
2 (20%) |
‒ |
2 (10%) |
|
Injury to major blood vessels |
‒ |
‒ |
‒ |
‒ |
|
Surgical site infection |
‒ |
1 (10%) |
1 (14%) |
2 (10%) |
|
Reoperation |
1 (25%) |
1 (10%) |
‒ |
2 (10%) |
Data have been obtained confirming the effectiveness of the author’s method of MIPIVS using distraction cages in patients with degenerative spondylolisthesis of the lumbar spine.
The significance of this approach lies in the ongoing search within spinal surgery for optimal treatment methods that combine effective deformity correction with segmental spinal stability while reducing the incidence of postoperative complications. Minimally invasive technologies, particularly the use of transpedicular fixation and interbody cages, are currently considered among the most promising directions in the surgical management of degenerative spinal disorders [17–19].
The results of our study demonstrated that patients in the study group, who underwent surgery using the author's technique, showed more pronounced positive dynamics in functional recovery compared to the standard treatment and control groups. Pre- and postoperative assessments revealed a significant reduction in pain intensity on the VAS. In the study group, pain levels decreased by an average of 4 points, while in the comparison group the reduction was 3 points, and in the control group — 2 points (the differences were statistically significant). Furthermore, assessment of functional status using the Oswestry Disability Index (ODI) showed marked improvement in the main group (a reduction of 10 points), indicating more effective restoration of the spinal motion segment and minimal limitations in daily activities.
A critically important outcome is the restoration of intervertebral disc height following surgery, as this parameter is key to ensuring the stability and functionality of the spinal motion segment. In the study group, postoperative increase in intervertebral disc height averaged 10 [9;11] mm, which was higher than that observed in the comparison group (8 [5;9] mm, p<0.05). Restoration of disc height plays a decisive role in reducing nerve structure compression, thereby alleviating neurological deficits and pain symptoms. Another essential aspect is the preservation of spinopelvic balance, a major factor in achieving a sustained positive clinical outcome. According to the collected data, the correction of sacral and pelvic tilt angles was most optimal in the main group, further supporting the effectiveness of the applied technique in ensuring biomechanical stability.
The assessment of intraoperative parameters demonstrated that the use of distraction cages significantly reduced the duration of the surgical procedure and hospitalization, as well as the volume of blood loss. The average operative time in the study group was 180 [180;180] minutes, which aligns with the standard parameters for MIS-PLIF (minimally invasive surgery posterior lumbar interbody fusion) and was significantly shorter (p<0.05) compared to the control group, where the operative time was 360 [240;480] minutes. The reduction in operative time directly contributes to a decreased risk of intraoperative complications such as blood loss and infectious complications. Intraoperative blood loss in the study group was considerably lower—100 [100;100] ml—compared to the comparison group, which recorded 200 [200;300] ml (p<0.05), and the control group, where blood loss amounted to 500 [400;600] ml (p<0.05). This reduction minimizes the need for blood transfusions and lowers the risk of hypovolemic shock.
An analysis of postoperative complications revealed the lowest incidence in patients treated using the authors’ proprietary technique. Specifically, no cases of paravertebral muscle atrophy were observed in the study group, while the incidence in the comparison group was 100% and 50% in the control group (p<0.05). This outcome is attributed to the fundamentally different surgical access technique, indicating that the minimally invasive approach significantly reduces the risk of iatrogenic damage to the musculo-ligamentous apparatus and promotes improved postoperative recovery.
The rate of postoperative bleeding was 27% and 33% in the comparison and control groups, respectively, whereas no such cases were observed in the main group (p<0.05). A significant reduction in the risk of radiculitis with spinal nerve root dysfunction was also of clinical importance. This complication occurred in only 25% of cases in the main group, compared to 30% in the comparison group and 50% in the control group (p<0.05).
These findings are consistent with contemporary studies demonstrating the advantages of minimally invasive techniques in the treatment of degenerative spondylolisthesis. Such methods reduce the risk of surgical complications, improve postoperative outcomes, and shorten the rehabilitation period. In particular, significant improvement in sagittal balance parameters has been observed in patients who underwent treatment with distraction cages within the MIS-PLIF framework [20, 21].
Conclusions
Prospects for further research
Clinical validation of minimally invasive posterior interbody stabilization using distraction cages in patients with lumbar spondylolisthesis is planned.
Disclosure
Conflict of Interest
The authors declare no conflict of interest.
Ethical Standards
All procedures performed on patients in the course of this study complied with the ethical standards of the institutional and national research ethics committees and with the 1964 Helsinki Declaration and its subsequent amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Funding
The research received no external funding.
Acknowledgements
The authors express their gratitude to the administration of the Municipal Non-Profit Enterprise of the Kharkiv Regional Council "Regional Clinical Hospital", Kharkiv National Medical University, and the Prof. M. I. Sitenko Institute of Spine and Joint Pathology of the National Academy of Medical Sciences of Ukraine for the opportunity to conduct this research based on their facilities; to LLC “Kalmykov Consulting” for assistance in systematizing the results of the clinical research phase; and to all colleagues for their constructive discussion, validation, and implementation of the findings.
References
1. García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Acta Ortop Mex. 2020 Sep-Oct;34(5):324-328. English.
2. Chung CC, Shimer AL. Lumbosacral Spondylolysis and Spondylolisthesis. Clin Sports Med. 2021 Jul;40(3):471-490. https://doi.org/10.1016/j.csm.2021.03.004
3. Bydon M, Alvi MA, Goyal A. Degenerative Lumbar Spondylolisthesis: Definition, Natural History, Conservative Management, and Surgical Treatment. Neurosurg Clin N Am. 2019 Jul;30(3):299-304. https://doi.org/10.1016/j.nec.2019.02.003
4. García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpízar-Aguirre A, Reyes-Sánchez A. Lumbar degenerative spondylolisthesis II: treatment and controversies. Acta Ortop Mex. 2020 Nov-Dec;34(6):433-440. English.
5. Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye AD. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(3):36917. https://doi.org/10.52965/001c.36917
6. Arts MP, Wolfs JF, Kuijlen JM, de Ruiter GC. Minimally invasive surgery versus open surgery in the treatment of lumbar spondylolisthesis: study protocol of a multicentre, randomised controlled trial (MISOS trial). BMJ Open. 2017 Nov 12;7(11):e017882. https://doi.org/10.1136/bmjopen-2017-017882
7. Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res. 2019 Jul 22;14(1):229. https://doi.org/10.1186/s13018-019-1266-y
8. Lu VM, Kerezoudis P, Gilder HE, McCutcheon BA, Phan K, Bydon M. Minimally Invasive Surgery Versus Open Surgery Spinal Fusion for Spondylolisthesis: A Systematic Review and Meta-analysis. Spine (Phila Pa 1976). 2017 Feb;42(3):E177-E185. https://doi.org/10.1097/BRS.0000000000001731
9. Ntoukas V, Müller A. Minimally invasive approach versus traditional open approach for one level posterior lumbar interbody fusion. Minim Invasive Neurosurg. 2010 Feb;53(1):21-4. https://doi.org/10.1055/s-0030-1247560
10. Yang Y, Liu ZY, Zhang LM, Pang M, Chhantyal K, Wu WB, Chen ZH, Luo CX, Rong LM, Liu B. Microendoscopy-Assisted Minimally Invasive Versus Open Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Diseases: 5-Year Outcomes. World Neurosurg. 2018 Aug;116:e602-e610. https://doi.org/10.1016/j.wneu.2018.05.049
11. Schnake KJ, Fleiter N, Hoffmann C, Pingel A, Scholz M, Langheinrich A, Kandziora F. PLIF surgery with titanium-coated PEEK or uncoated PEEK cages: a prospective randomised clinical and radiological study. Eur Spine J. 2021 Jan;30(1):114-121. https://doi.org/10.1007/s00586-020-06642-x
12. Nekhlopochyn O, Verbov V, Tsymbaliuk I, Cheshuk I, Vorodi M. The choice of classification to determine the optimal tactics for treatment of the thoracolumbar junction traumatic injuries. Pol Merkur Lekarski. 2024;52(1):104-111. https://doi.org/10.36740/Merkur202401116
13. Ashworth E, Baxter D, Gibb I, Wilson M, Bull AMJ. Injuries in Underbody Blast Fatalities: Identification of Five Distinct Mechanisms of Head Injury. J Neurotrauma. 2023 Jan;40(1-2):141-147. https://doi.org/10.1089/neu.2021.0400
14. Pereira P, Park Y, Arzoglou V, Charles YP, Krutko A, Senker W, Park SW, Franke J, Fuentes S, Bordon G, Song Y, He S, Vialle E, Mlyavykh S, Varanda P, Hosszu T, Bhagat S, Hong JY, Vanhauwaert D, de la Dehesa P. Anterolateral versus posterior minimally invasive lumbar interbody fusion surgery for spondylolisthesis: comparison of outcomes from a global, multicenter study at 12-months follow-up. Spine J. 2023 Oct;23(10):1494-1505. https://doi.org/10.1016/j.spinee.2023.05.013
15. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015 Dec;1(1):2-18. https://doi.org/10.3978/j.issn.2414-469X.2015.10.05
16. Stognii A, Pyatikop V, Yaresko O, Popsuyshapka K, Pidgayska O, Karpinsky M. [Study of stress distribution in the posterior lumbar interbody fusion model (PEEK implant and distraction cage)]. TRAUMA. 2022;23(6):47-55. Ukrainian. https://doi.org/10.22141/1608-1706.6.23.2022.923
17. Arim O, Alshalcy A, Shakir M, Agha O, Alhamdany H. TRANSPEDICULAR SCREW FIXATION IN DEGENERATIVE LUMBOSACRAL SPINE DISEASE SURGICAL OUTCOME. Georgian Med News. 2024 Mar;(348):117-121
18. Doğu H, Abdallah A, Muçuoğlu AO, Demirel N, Elmadağ NM. Comparing Three-dimensional and Two-dimensional Preoperative Planning for Lumbar Transpedicular Screw Placement: A Retrospective Study. J Neurol Surg A Cent Eur Neurosurg. 2025 Jan;86(1):1-11. https://doi.org/10.1055/a-2175-3215
19. Wu L, Jiang X, Guan T, He Z, Li J. Biomechanical properties analysis of posterior lumbar interbody fusion with transpedicular oblique screw fixation. Heliyon. 2024 Oct 4;10(19):e38929. https://doi.org/10.1016/j.heliyon.2024.e38929
20. Lewandrowski KU, Soriano-Sánchez JA, Zhang X, Ramírez León JF, Soriano Solis S, Rugeles Ortíz JG, Martínez CR, Alonso Cuéllar GO, Liu K, Fu Q, de Lima E Silva MS, de Carvalho PST, Hellinger S, Dowling Á, Prada N, Choi G, Datar G, Yeung A. Surgeon motivation, and obstacles to the implementation of minimally invasive spinal surgery techniques. J Spine Surg. 2020 Jan;6(Suppl 1):S249-S259. https://doi.org/10.21037/jss.2019.08.02
21. Modi HN, Shrestha U. Comparison of Clinical Outcome and Radiologic Parameters in Open TLIF Versus MIS-TLIF in Single- or Double-Level Lumbar Surgeries. Int J Spine Surg. 2021 Oct;15(5):962-970. https://doi.org/10.14444/8126