Case Report
Ukrainian Neurosurgical Journal. 2025;31(1):55-60
https://doi.org/10.25305/unj.319976
1 Panchakarma, Manjushree Research Institute of Ayurvedic Science, Gandhinagar, India
2 Panchakarma, Datta Meghe Institute of Higher Education and Research Wardha, Maharashtra, India
3 Agadtantra, Manjushree Research Institute of Ayurvedic Science, Gandhinagar, India affiliated to Gujarat Ayurved University, Jamnagar, India
Received: 01 January 2025
Accepted: 14 January 2025
Address for correspondence:
Satyajit P. Kulkarni, Manjushree Research Institute of Ayurvedic Science, Gandhinagar, 382610, India, e-mail: satyajitkulkarni2001@gmail.com
This case report details the Ayurvedic treatment of a 49-year-old male with gait difficulties and pain due to lumbar canal stenosis. A three-week course of Ayurvedic therapies, including massage and oral medications, resulted in significant pain reduction (low back pain VAS from 5 to 2; leg pain from 6 to 2) and improvement in the straight leg raise test (40 to 60 degrees). While some gait parameters showed minimal change (step length 0.70m to 0.69m; stride length unchanged; step time 0.48s to 0.49s; stride time unchanged), walking speed increased (1.24 m/s to 1.39 m/s) and gait asymmetry decreased (22% to 20%). While suggesting potential benefits of Ayurveda for pain management in lumbar canal stenosis, the limited impact on gait parameters underscores the need for further research, including objective gait analysis and controlled studies, to confirm efficacy.
Keywords: sciatica; lumbar spinal stenosis; intermittent neurogenic claudication; gait disorder; case report; Ayurveda
Introduction
Gait disorders significantly impact an individual's quality of life, affecting daily activities and increasing fall risk [1]. Intermittent Neurogenic Claudication (INC), a common symptom of Degenerative Lumbar Spinal Stenosis (DLSS), often manifests as leg pain, numbness, and lower back pain, contributing to gait disturbances [2]. While the exact pathophysiology of INC in DLSS remains unclear, it is postulated that reduced intervertebral disc nutrition plays a critical role. This impaired gait can significantly diminish an individual's mobility and overall well-being [3].
Ayurveda, the traditional Indian system of medicine, offers a holistic approach to managing such conditions by emphasizing the restoration of balance and harmony within the body [4-5]. Although, conventional treatments for DLSS and associated gait disorders exist, some individuals seek complementary or alternative therapies like Ayurveda. However, there is limited research specifically exploring the efficacy of Ayurvedic interventions for gait disorders secondary to INC. This case report presents the Ayurvedic management of a patient experiencing gait disturbance due to INC, aiming to contribute to the existing literature on this topic [6-7].
The patient, a 49-year-old male, presented with difficulty walking and an unsteady gait. Initial evaluation revealed no apparent neurological deficits; however, the patient reported imbalance and decreased confidence in ambulating. An Ayurvedic assessment identified an imbalance in the patient's Vata dosha, the principle governing movement and nervous system function. The treatment plan incorporated herbal remedies, lifestyle modifications, and targeted Panchakarma therapy. The patient's progress was closely monitored, with adjustments to the treatment plan as needed. Over time, the patient demonstrated significant improvements in gait and balance, regaining confidence in performing daily activities.
Case Presentation
A 49-year-old male presented with unsteady gait and instability following episodes of lower back pain and leg cramps. Initial neurological examination was unremarkable, however, the patient reported subjective imbalance and decreased confidence in ambulation. The patient's pain was assessed using a numerical rating scale (NRS), with reported pain intensity of 6/10 in the lower back and 5/10 in the left leg.
The patient also exhibited difficulty maintaining an erect posture while standing and walking. The pain intensified after ambulating approximately 50 meters and was relieved by assuming a seated position.
Additionally, the patient experienced paraesthesia in the left lower extremity. Symptom exacerbation was noted during the winter months. The patient's primary concerns were the onset of leg pain after ambulating short distances and postural instability.
The patient, of low socioeconomic status, is the primary provider and sole wage earner for his family. His occupation involves driving a private passenger van between Gandhinagar and neighbouring towns, often under overcrowded conditions requiring prolonged driving in an uncomfortable posture. In addition to this occupation, he engages in various forms of manual labour in his rural community. The patient has a history of tobacco use including tobacco products for over 10 years. The patient's medical history is unremarkable for trauma, hypertension, diabetes, psychiatric illness, vascular disease, Pott's disease, or arthritis.
He initially sought treatment at a government hospital orthopaedic clinic, where he received nonsteroidal anti-inflammatory drugs (NSAIDs) and physiotherapy for 15 days. Four months later, upon recurrence of symptoms, spinal decompression surgery was recommended. However, due to financial constraints and inability to take leave from work for postoperative recovery, the patient opted to manage pain exacerbations with NSAIDs (Table 1).
Table 1. Timeline of symptoms
|
Year |
Symptoms |
|
2017 |
The patient initially presented with lower back pain and leg pain, which responded to NSAIDs prescribed by an orthopaedic specialist. |
|
2019 |
Symptom severity increased, with the patient experiencing postural instability during walking and standing. Spinal surgery was recommended but deferred due to financial constraints. |
|
2023 |
The patient, referred by a relative, sought alternative treatment at our facility. |
The patient presented to our hospital accompanied by a relative and agreed to Ayurvedic treatment after being assured of affordable care. Physical examination revealed a medium-built individual (height 162.56 cm, weight 57 kg) with normal vital signs. The straight leg raise (SLR) test was positive at 45 degrees for the left leg, accompanied by hyperreflexia in the left foot. The SLR and reflexes were normal in the right leg. Dorsalis pedis and posterior tibial pulses were palpable and normal bilaterally. The patient demonstrated an abnormal gait and experienced leg cramps after ambulating for 10-15 minutes. The pain was absent during spinal flexion and while seated.
Based on accompanying medical records, the patient had been diagnosed with lumbar spinal stenosis with intermittent neurogenic claudication by an orthopedic consultant, attributed as the cause of the patient's pain and gait abnormalities. While the records indicated prior analgesic medication and a recommendation for spinal surgery, imaging studies were not available for review. The initial pain episode occurred six years prior. Subsequent gait abnormalities and progressive restriction of movement developed over the following 2-3 years, with the current condition remaining stable for the past year.
An Ayurvedic assessment identified a Vata dosha imbalance. Vata is the principle governing movement and nervous system function. The patient's pain radiated from the gluteal region to the upper and lower back, knee, and sole of the left foot, consistent with the Ayurvedic diagnosis of Ghridhrasi. Furthermore, the patient's gait exhibited a vulture-like limp, further supporting this diagnosis with a Vata-dominant subtype (Fig. 1, Fig. 2, Fig. 3).
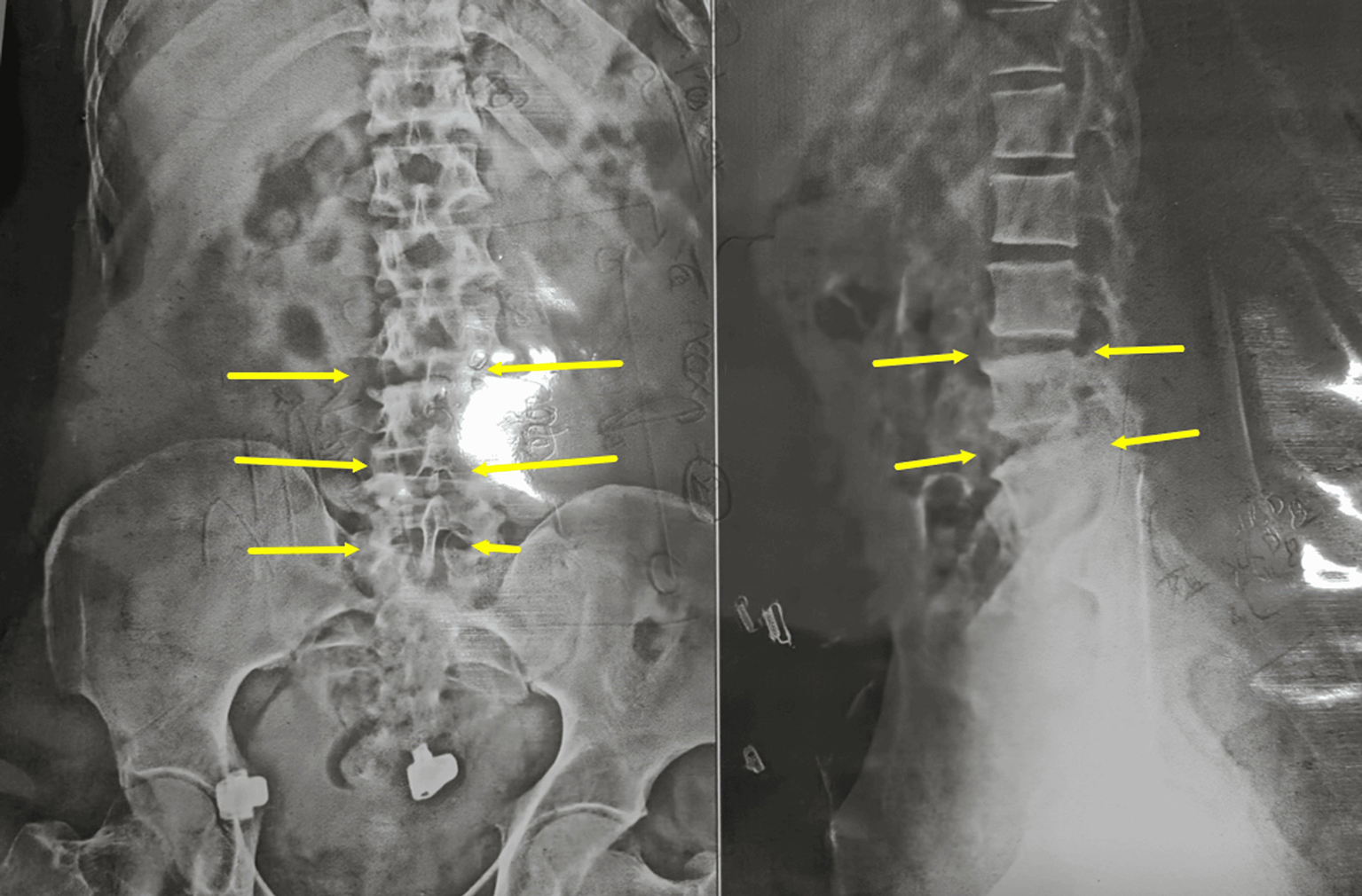
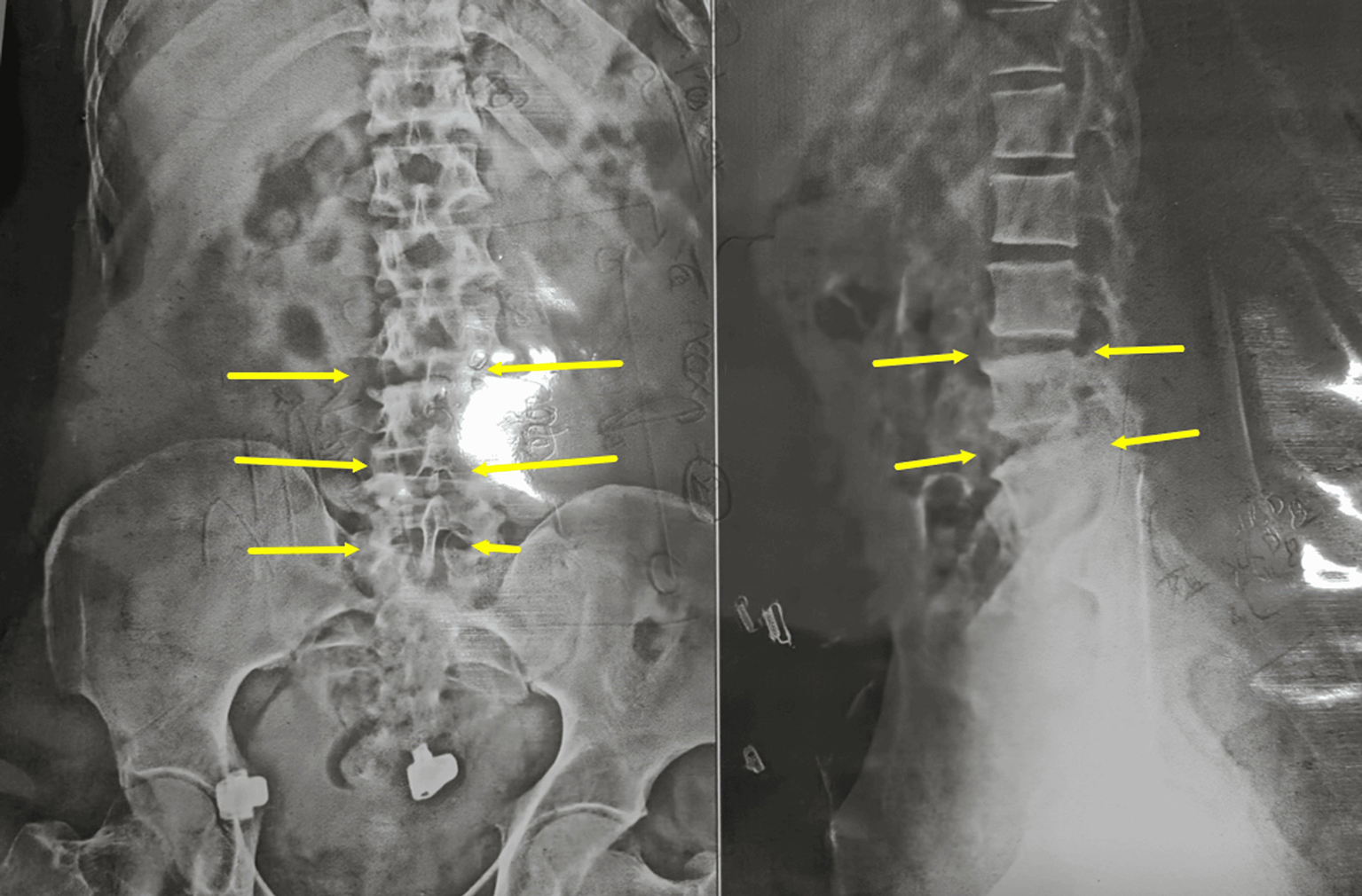
Fig. 1. X-ray of the Lumbar spine (AP view) showing degenerative changes from L3 to S1
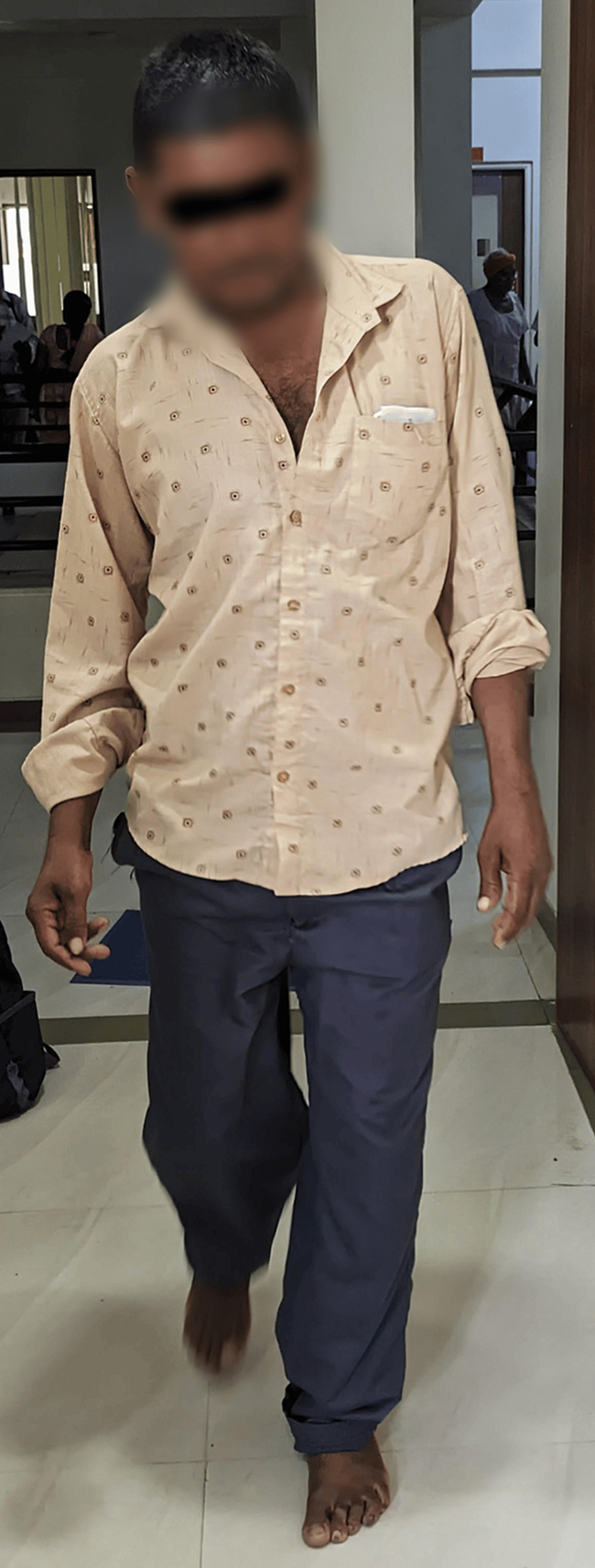
Fig. 2. Gait view anteriorly before treatment
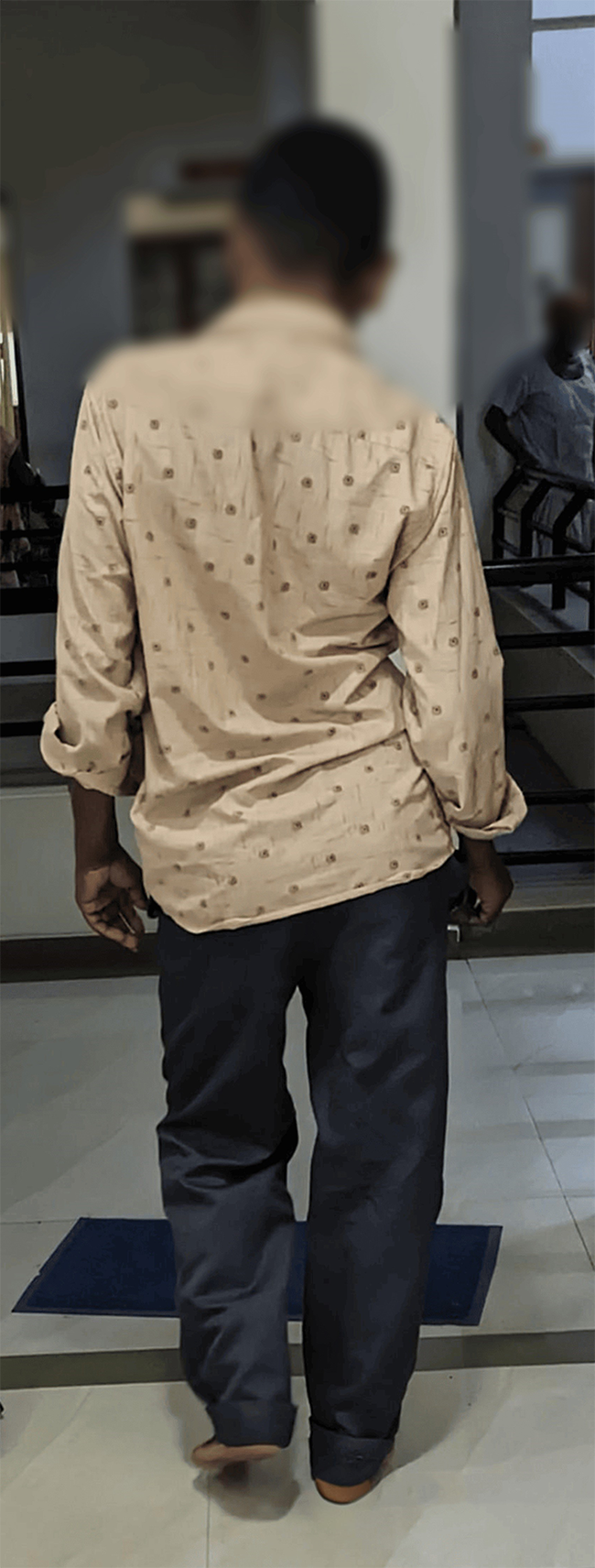
Fig. 3. Gait view posteriorly before treatment
Based on the Ayurvedic diagnosis, a treatment plan was implemented consisting of Panchakarma therapies, oral Ayurvedic medications, and dietary modifications. Informed consent was obtained prior to the initiation of Panchakarma procedure.
Abhyanga (oil massage) was performed to the whole body by two practitioners for 30-45 minutes using lukewarm sesame oil.
Swedana (heat therapy) was administered following massage. The patient was seated in a wooden cabinet connected to a steam generator containing vaporized Ayurvedic decoctions. This treatment was administered for 10 minutes to induce full-body sweating. Ayurvedic management involved a comprehensive assessment of the patient's prakriti (constitutional type) and Dosha imbalance. The treatment plan incorporated herbal remedies, lifestyle modifications, and targeted physical therapy.
Oral Ayurvedic medicines
Trayodashang Guggulu, a classical Ayurvedic polyherbal formulation officially listed in the Ayurvedic Formulary of India and Ayurvedic Pharmacopoeia of India, was prescribed. Traditionally indicated for conditions such as arthritis, lumbar-sacral and knee stiffness, sciatica, arm pain, ligament injuries, and fractures. This formulation contains 13 herbs in addition to Guggul, Babula, Ashwagandha, Hapusa, Guduchi, Shatavari, Gokshuara, Vradadaru, Rasana, Satavha, Sati, Yavani, Sunthi, and Goghrat (ghee). The patient was prescribed 250 mg three times daily with warm water before breakfast and after lunch and dinner.
Sinhanad Guggulu, containing Trifala (a combination of Emblica officinalis, Terminalia chebula, and Terminalia bellirica), guggul, Gandhak (sulfur), and Erandamool, was also prescribed for lower back pain, disability, and leg pain, following the same dosage regimen as Trayodashang Guggulu.
Dashmool Kwatha, a decoction prepared from ten herbs, was also administered. A freshly prepared decoction was provided by the hospital pharmacy.
Duration of the treatment lasted 3 weeks.
An Ayurvedic diet was prescribed. The patient was instructed to ambulate each morning within the hospital premises under nursing staff supervision, recording the distance covered. The patient was instructed to ambulate to the limit of his comfort level.
The patient's progress was monitored closely, and adjustments were made to the treatment plan as needed. Over time, the patient's gait and balance improved significantly, and he regained his confidence in performing daily activities.
The patient was assessed according to the following parameters:
Pain intensity for both low back pain and leg pain was assessed using the Visual Analogue Scale (VAS). Patients rated their pain on a 0-10 scale (0 = no pain, 10 = worst imaginable pain). VAS scores were recorded before and after the treatment periods.
Lumbar radiculopathy was assessed using the Extended Straight Leg Raise (ESLR) Test. A positive test, indicated by radiating pain down the affected leg during passive hip flexion with knee extension (particularly at angles less than 45 degrees), suggests L5 or S1 nerve root involvement. ESLR was assessed before and after the treatment periods.
Ambulation distance, measured as a functional outcome, was assessed by instructing the patient to walk at a comfortable pace to the limit of their tolerance. Walking distance was recorded before and after the treatment periods.
Gait examination - A stride, or gait cycle, is defined as two consecutive steps, completing a full cycle of foot movement. Each gait cycle consists of stance phase (foot in contact with the ground) and swing phase (foot off the ground, moving forward). Gait analysis can further evaluate double support time (both feet in contact with the ground) and single support time (one foot in contact with the ground). These phases can be expressed as percentages of the gait cycle and compared to normative values: stance (60%), swing (40%), and double support time (20%) [8] (Fig. 4, Fig. 5).

Fig. 4. Gait view anteriorly after treatment

Fig. 5. Gait view posteriorly after treatment
Spatial and temporal gait parameters were collected. [9]
Spatial Parameters
Step Length: Average distance between consecutive foot contacts (meters).
Stride Length: Average distance between consecutive contacts of the same foot (meters).
Temporal Parameters
Step Time: Average time between consecutive foot contacts (seconds).
Stride Time: Average time between consecutive contacts of the same foot (seconds).
Walking Speed: Average distance traveled per second (meters/second).
Cadence: Average number of steps per minute.
Step Time Asymmetry: Average difference in step time between left and right feet (seconds) (Table 2).
Table 2. Observations before and after treatment
|
Parameter |
BT |
AT |
|
Low back pain (VAS) |
5 |
2 |
|
Leg pain (VAS) |
6 |
2 |
|
SLR Test positive |
40 degrees |
60 degrees |
|
Step length |
0.70 m |
0.69 m |
|
Stride length |
72 cm |
72 cm |
|
Step Time |
0.48 sec |
0.49 sec |
|
Stride Time |
0.98 sec |
0.98 sec |
|
Walking speed |
1.24 m/s |
1.39 m/s |
|
Cadence |
172/min |
180/min |
|
Step Time Asymmetry |
22% |
20% |
No changes were made to the patient's medications or procedures due to reported tolerance and the absence of adverse drug reactions.
Discussion
This case report describes the Ayurvedic management of a 49-year-old male patient with lumbar spinal stenosis and intermittent neurogenic claudication, presenting with abnormal gait, moderate lumbar pain, leg cramps, and severely limited walking distance. The patient received Ayurvedic massage and hot fomentation with herbal decoction daily for three weeks, without the use of conventional analgesics. The treatment resulted in marked improvement in pain and lumbar disability, with slight improvement in gait abnormalities.
Significant improvements were observed in both low back pain (reduced from 5 to 2) and leg pain (reduced from 6 to 2), likely attributable to the combined effects of Ayurvedic medications and Panchakarma therapies. The increased range of motion in the Straight Leg Raise Test (from 40 to 60 degrees) further suggests substantial relief from pain and muscle spasm following treatment.
Minimal changes were observed in most gait parameters with pre- and post-treatment values were as follows: step length (0.70 m to 0.69 m), stride length (72 cm to 72 cm), step time (0.48 sec to 0.49 sec), stride time (0.98 sec to 0.98 sec), walking speed (1.24 m/s to 1.39 m/s), cadence (172/min to 180/min), and step time asymmetry (22% to 20%). Improvements were noted in walking speed and step time asymmetry, potentially attributable to pain and spasm reduction facilitated by the Ayurvedic treatment.
While lumbar spinal stenosis with intermittent neurogenic claudication is typically managed with conventional medical interventions, including pharmacotherapy, physical therapy, and in some cases, surgery [10], this case highlights the potential of Ayurvedic approaches. The observed improvements in pain and function suggest that Ayurvedic massage and fomentation may offer a complementary or alternative approach for managing symptoms associated with lumbar spinal stenosis. The mechanisms by which these therapies exert their effects are not fully understood but may involve improved circulation, reduced muscle tension, and modulation of inflammatory processes [10].
It is important to note the limitations of this case report, including the small sample size (n=1) and the lack of a control group. These limitations preclude definitive conclusions about the efficacy of Ayurvedic treatment for lumbar spinal stenosis. Further research, including randomized controlled trials, is needed to rigorously evaluate the effectiveness and safety of these therapies. Additionally, the specific details of the Ayurvedic interventions, including the composition of the herbal decoction, could be further elaborated in future studies.
Conclusion
This case study suggests that a three-week course of Ayurvedic treatment may reduce pain and disability associated with lumbar spinal stenosis and intermittent neurogenic claudication, while also potentially improving gait disturbances. While prior research has explored the use of Ayurveda for spinal conditions like LSS, its impact on gait abnormalities stemming from INC in LSS patients remained to be investigated. Though Ayurveda may offer benefits for pain associated with lumbar canal stenosis, its limited effect on gait necessitates further investigation with objective gait analysis and controlled trials to establish clinical efficacy.
Disclosures
Human subjects
Consent was obtained or waived by all participants in this study.
Conflicts of interest
In compliance with the International Committee of Medical Journal Editors uniform disclosure form, all authors declare the following:
Payment/services info
All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships
All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships
All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements
Authors acknowledges the interns, teaching staff and hospital staff of Manjushree Research Institute of Ayurvedic Science, Piplaj for their support in treating this patient.
References
1. Axer H, Axer M, Sauer H, Witte OW, Hagemann G. Falls and gait disorders in geriatric neurology. Clin Neurol Neurosurg. 2010 May;112(4):265-74. https://doi.org/10.1016/j.clineuro.2009.12.015
2. Park JS, Koo SM, Kim CH. Classification of Standing and Walking States Using Ground Reaction Forces. Sensors (Basel). 2021 Mar 18;21(6):2145. https://doi.org/10.3390/s21062145
3. Ronthal M. Gait Disorders and Falls in the Elderly. Med Clin North Am. 2019 Mar;103(2):203-213. https://doi.org/10.1016/j.mcna.2018.10.010
4. Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007 Jan;6(1):63-74. https://doi.org/10.1016/S1474-4422(06)70678-0
5. Viswanathan A, Sudarsky L. Balance and gait problems in the elderly. Handb Clin Neurol. 2012;103:623-34. https://doi.org/10.1016/B978-0-444-51892-7.00045-0
6. Wasedar V, Pangam B, Shete S, Belaval V. Complete resolution of lumbar disc sequestration with Ayurveda management: A case report. J Ayurveda Integr Med. 2023 Nov-Dec;14(6):100826. https://doi.org/10.1016/j.jaim.2023.100826
7. Pandey VY, Kaushik N. Ayurvedic Management of Lumbar Disc disease-A Case Report. Ancient Science of Life. 2018 Jul 1;38(1):26-31. https://doi.org/10.4103/asl.ASL_197_17
8. Natarajan P, Fonseka RD, Kim S, Betteridge C, Maharaj M, Mobbs RJ. Analysing gait patterns in degenerative lumbar spine diseases: a literature review. J Spine Surg. 2022 Mar;8(1):139-148. https://doi.org/10.21037/jss-21-91
9. Haber CK, Sacco M. Scoliosis: lower limb asymmetries during the gait cycle. Arch Physiother. 2015 Jul 8;5:4. https://doi.org/10.1186/s40945-015-0001-1
10. Bussières A, Cancelliere C, Ammendolia C, Comer CM, Zoubi FA, Châtillon CE, Chernish G, Cox JM, Gliedt JA, Haskett D, Jensen RK, Marchand AA, Tomkins-Lane C, O'Shaughnessy J, Passmore S, Schneider MJ, Shipka P, Stewart G, Stuber K, Yee A, Ornelas J. Non-Surgical Interventions for Lumbar Spinal Stenosis Leading To Neurogenic Claudication: A Clinical Practice Guideline. J Pain. 2021 Sep;22(9):1015-1039. https://doi.org/10.1016/j.jpain.2021.03.147