
Original article
Ukrainian Neurosurgical Journal. 2025;31(2):37-43
https://doi.org/10.25305/unj.318996
1 Department of Medicine, Kherson State University, Ivano-Frankivsk, Ukraine
2 Medical center "Family Medicine Clinic", Dnipro, Ukraine
Received: 25 December 2024
Accepted: 17 February 2025
Address for correspondence:
Oleg M. Tarasenko, Department of Medicine, Kherson State University, 57 Shevchenko St., Ivano-Frankivsk, 76018, Ukraine, e-mail: tarasenko_om@i.ua
More than 800,000 microdiscectomies are performed annually worldwide. According to various authors, good and excellent results are about 85%, with adequate selection of patients for surgical treatment. Nevertheless, up to 40% of patients continue to suffer from pain, motor and sensory disorders, although their intensity decreases after surgery. Therefore, the search for new methods of surgical interventions that will improve the results of treatment of such patients continues.
In the late 90s of the last century, the JOIMAX company (Germany) developed a technique for endoscopic transforaminal microdiscectomy, which used a lateral (transforaminal) rather than a standard interlaminar approach. According to literature data, endoscopic transforaminal microdiscectomy has up to 93% of positive outcomes.
Objective: To study the immediate and long-term outcomes of treatment of patients with herniated intervertebral discs in the lumbar spine using the transforaminal endoscopic microdiscectomy method.
Materials and methods: The immediate (1st day after surgery) and long-term (6th month postoperatively) outcomes of surgical treatment of 68 patients with herniated intervertebral discs in the lumbar spine were studied. Patients were operated on using the endoscopic transforaminal microdiscectomy method at the «Family Medicine Clinic», Dnipro from 2020 to 2024.
Results: There were 52 men and 16 women, the age of the patients ranged from 24 to 68 years (average 44.2 years), the duration of the disease was from 6 months to 12 years. Before the operation, the average pain score according to VAS was 8.7 points. Pain syndrome on the VAS scale on the 1st day after surgery was, on average, 3.5 points, after 6 months - 3 points. After 6 months after surgery, 63 patients (93%) had good treatment outcomes according to the J. MacNab scale. Unsatisfactory results were in 5 patients (7%).
Conclusions: Transforaminal endoscopic microdiscectomy is a modern highly effective minimally invasive method of surgical treatment of herniated intervertebral discs in the lumbar spine, which allows to significantly reduce intraoperative trauma, the patient’s hospital stay, accelerate the rehabilitation of patients, and improve treatment outcomes.
Keywords: transforaminal endoscopic microdiscectomy; minimally invasive treatment methods; outpatient neurosurgery
Introduction
It is estimated that more than 800,000 microdiscectomies are performed annually worldwide [1]. According to various authors, the rate of good to excellent outcomes reaches approximately 85% when patients are appropriately selected for surgical treatment; however, around 40% of patients continue to experience pain, motor, and sensory disturbances, albeit with reduced intensity postoperatively [1, 2, 4]. Unsatisfactory treatment outcomes are classified under the so-called "failed back surgery syndrome" (FBSS). Postoperative compressive scar-adhesive epiduritis—a reactive productive inflammatory process that invariably develops after surgical interventions (including microdiscectomies)—accounts for about 25% of FBSS cases [2]. According to different sources, FBSS is responsible for approximately 20% of repeat surgeries. Although microdiscectomy continues to be considered the gold standard, over the past 30 years, numerous new techniques and their modifications have been proposed. The developers of these methods aim to minimize the trauma associated with surgical access while maintaining the radical nature of the operation [1, 2]. The ongoing search for new surgical techniques focuses on reducing intraoperative trauma, shortening hospital stays, decreasing the frequency of postoperative complications, improving treatment outcomes, accelerating patient rehabilitation, and lowering treatment costs.
The predominant trend is the enhancement of the micro-surgical interlaminar approach, particularly through the development of retractors that minimize damage to the paravertebral muscles. Additionally, minimally invasive approaches to herniated discs have been proposed that avoid the removal of the ligamentum flavum and additional facetectomy [3–7]. A major drawback of the posterior interlaminar approach is that, after incision or resection of the ligamentum flavum, the surgeon sees the nerve root and dural sac in the wound, while the herniation is typically located posterior to these structures; thus, its removal requires traction of both the nerve root and the dural sac [5, 8–11]. Alongside advancements in microsurgical techniques, endoscopic methods have been introduced to reduce access-related trauma. The most widely used method in the 1990s was endoscopic monoportal or biportal nucleotomy, which was successfully applied not only in the treatment of disc protrusions and small hernias but also in sequestrated herniations [4–9]. However, this method lacked the versatility of microdiscectomy and often necessitated repeat surgical interventions.
At the end of the 1990s, the German company "Joimax" developed a technique for endoscopic microdiscectomy that used a lateral (transforaminal) approach instead of the standard interlaminar one. In this procedure, the surgeon enters the spinal canal laterally through the intervertebral foramen. This allows for the herniated disc to be visualized first, followed by the nerve root. With this approach, nerve root traction is not required. The TESSYS (Transforaminal Endoscopic Surgical System) technique has gained widespread adoption across Europe [7–11]. The instruments used in this procedure are continually being refined, thereby expanding the capabilities of the technique. Numerous studies by international authors indicate the high efficacy of endoscopic transforaminal microdiscectomy and a low incidence of failures and complications. According to published data, endoscopic transforaminal microdiscectomy achieves approximately 93% positive outcomes, which is comparable to the efficacy of traditional "open" microdiscectomy [10–17]. Endoscopic transforaminal microdiscectomy offers several important advantages: the skin incision is only 5 mm long and typically heals without any cosmetic defect; muscles and aponeuroses are not incised but rather gently separated using tubular dilators; the maximum port diameter is 7.5 mm; and the absence of oxygen exposure reduces the risk of postoperative compressive scar-adhesive epiduritis. Hospitalization time does not exceed 12–20 hours, and the patient is mobilized three hours after surgery. These features qualify the technique as a form of "ambulatory neurosurgery", as a significant number of patients are discharged on the same day the operation is performed. The rehabilitation period is three times shorter than that following conventional microdiscectomy. However, some authors argue that the method is insufficiently radical and not universally applicable [11–15, 19].
Objective: To investigate the short- and long-term outcomes of treating patients with lumbar intervertebral disc herniation using transforaminal endoscopic microdiscectomy.
Materials and Methods
Study design
A single-center retrospective and prospective controlled study was conducted involving 68 patients. The medical records of 52 patients who underwent transforaminal endoscopic microdiscectomy between 2020 and 2024 were analyzed. The prospective arm of the study, comprising 16 patients, was conducted in 2024.
Study participants
The participants were patients with lumbar intervertebral disc herniations who underwent surgery at the "Family Medicine Clinic" (Dnipro, Ukraine).
The study was approved by the Biomedical Ethics Committee of Kherson State University (Minutes No. 7 dated June 30, 2024).
Inclusion Criteria
Patients with foraminal, posterolateral, or paramedian herniations in the lumbar spine who had completed a 4-week course of conservative therapy without positive effect.
Exclusion Criteria
Pre-defined limitations of the method included central disc herniations, foraminal stenosis, nerve root exit through the inferior aspect of the foramen, cranial migration of L5-S1 herniation, and life-threatening contraindications.
Analyzed parameters
Sex and age of the patient, duration of the disease, level, size, and location of the herniation, evaluation of outcomes using the Visual Analog Scale (VAS) and the modified J. MacNab scale.
Surgical technique
The procedure was performed under intravenous anesthesia with local potentiation. Muscle relaxant solutions were not used, which is essential for this type of surgery. The patient was placed in a prone position. The level of surgical intervention was verified using intraoperative radiography. The surgical approach is crucial to the success of the procedure; depending on the level of intervention, the distance from the midline increases in the caudal direction (Fig. 1). The operation can be conventionally divided into three stages:

Fig. 1. Indentation from the midline depending on the level of intervention

Fig. 2. Entry point for endoscope port placement

Fig. 3. Endoscope port placement

Fig. 4. Endoscope photo
After the operation is completed, one or two sutures are applied to the skin.
Statistical analysis
Statistical processing of the research data was performed using Python v3.9.5 (https://www.python.org/downloads) in the JupyterLab development environment (https://jupyter.org/install). Comparisons between independent groups were conducted using Fisher's exact test. The error threshold was set at p < 0.0001. A value of p < 0.0001 was considered critically significant for all types of analysis performed.
Results and discussion
Patient characteristics
The short-term (first postoperative day) and long-term (6 months after surgery) outcomes of surgical treatment were studied in 68 patients with lumbar intervertebral disc herniation. The patient was examined either upon discharge from the hospital or during wound dressing (for those discharged on the day of surgery), and again during a scheduled follow-up consultation six months later. Surgical outcomes were evaluated using the VAS and the modified J. MacNab scale. This methodology is routinely used at the "Family Medicine Clinic" (Dnipro) for the removal of paramedian, posterolateral, and foraminal hernias in the lumbar spine.
Among the patients, there were 52 men and 16 women aged 24 to 68 years (mean age – 44.2 years). The duration of the disease ranged from 6 months to 12 years. In all cases, conservative treatment methods, including physiotherapy and sanatorium-resort therapy for a period of no less than 4 weeks, failed to yield the desired results. All patients underwent magnetic resonance imaging (MRI) during the preoperative period.
Indications for surgical intervention included persistent lumbosciatic syndrome, sensory disturbances, moderate to severe motor deficits, and reflex impairments, combined with ineffective conservative therapy lasting at least 4 weeks and confirmed by morphological signs such as MRI-proven disc herniation. Surgical interventions were performed in the presence of neurocompressive syndromes caused by paramedian, posterolateral, or foraminal hernias (median hernias and L5–S1 hernias with cranial migration were removed as previously described).
The size of the foraminal opening and the location where the nerve root exits through it (Fig. 5) [18] are of crucial importance. To enlarge the foramen and place the endoscopic port, it is necessary to preserve the anatomical structure of the foraminal opening. If the nerve root exits through its upper portion, and the lower part, even in the presence of stenosis, still has space for placing a guidewire, the intervention can be successfully performed. However, if the root exits through the lower portion of the foramen or there is significant stenosis due to spondyloarthrosis, developmental anomalies, or pronounced spondylolisthesis, the operation will be unsuccessful—except in cases of foraminal hernias, where foramen opening is not required.
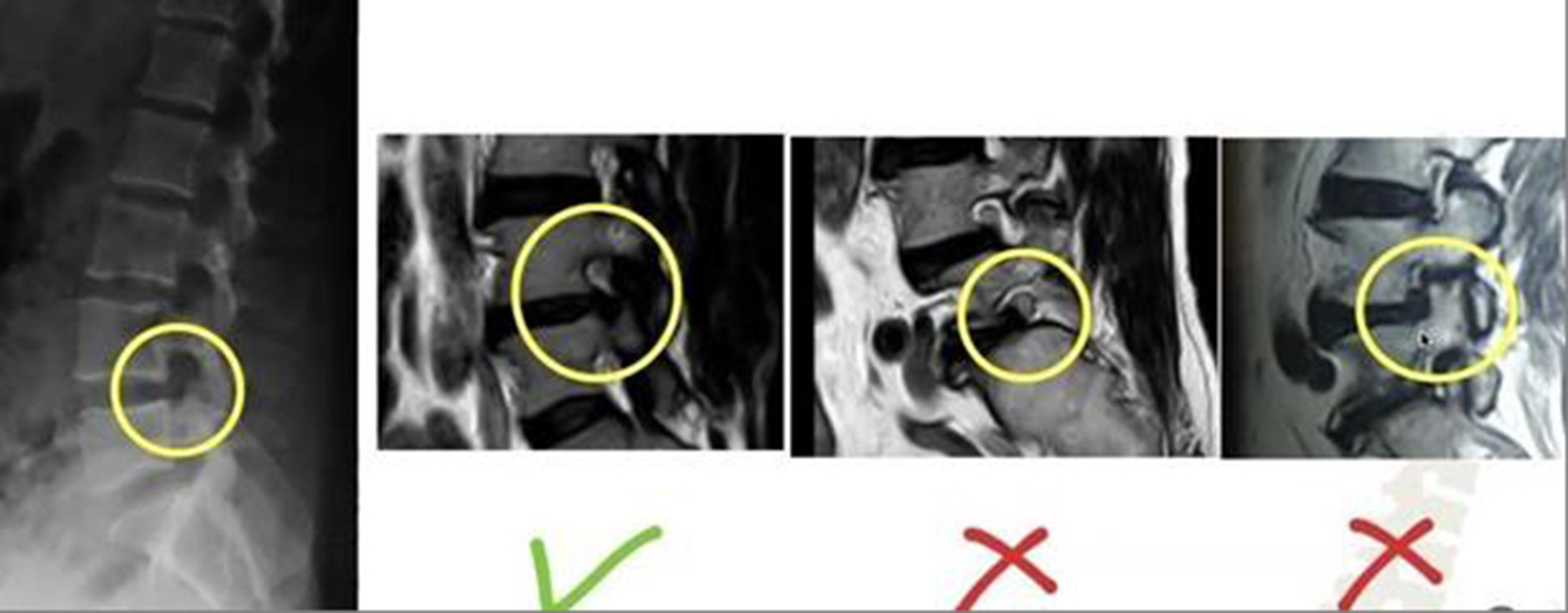
Fig. 5. Possibility of intervention depending on the size of the foraminal opening and the location of the nerve root (https://doi.org/10.1002/ca.22286)
Herniated discs at the L2–L3 level were detected in 5 patients (7%), at L3–L4 in 2 patients (3%), at L4–L5 in 35 patients (52%), and at L5–S1 in 26 patients (38%). Paramedian hernias were diagnosed in 21 cases (31%), posterolateral in - 39 cases (57%), and foraminal - in 8 cases (12%) (Table 1).
Table 1. Distribution of cases according to type and level of herniation
|
Level |
Type of hernia |
Total |
||
|
Paramedian |
Posterolateral |
Foraminal |
||
|
L2-L3 |
0 |
2 (3,0%) |
3 (4,0%) |
5 (7,0%) |
|
L3-L4 |
0 |
1 (1,5%) |
1 (1,5%) |
2 (3,0%) |
|
L4-L5 |
12 (18,0%) |
21 (31,0%) |
2 (3,0%) |
35 (52,0%) |
|
L5-S1 |
9 (13,0%) |
15 (22,0%) |
2 (3,0%) |
26 (38,0%) |
According to MRI data, in 32 cases (47%) the hernias measured up to 8 mm, while in 36 cases (53%) they exceeded 8 mm.
Treatment outcomes
Before surgery, the average pain score on the VAS was 8.7 points. On the first day after surgery, it decreased to 3.5 points, and six months later, it was 3.0 points (p < 0.0001 compared to the preoperative score).
Six months after the surgical intervention, 63 patients (93%) demonstrated good or satisfactory treatment outcomes according to the J. MacNab scale, while 5 patients (7%) had unsatisfactory results (Table 2).
Table 2. Evaluation of treatment outcomes using the J. MacNab scale six months after surgery
|
Results |
Number of observations |
|
|
Abs. |
% |
|
|
Good |
51* |
75 |
|
Satisfactory |
12 |
18 |
|
Unsatisfactory |
5 |
7 |
|
Total |
68 |
100 |
Note. * – The difference is statistically significant (p < 0.0001) compared to the indicator in patients with an unsatisfactory outcome.
Clinical Case
Patient H., a 53-year-old female, was hospitalized at the "Family Medicine Clinic" Medical Center on May 27, 2024, with the diagnosis of a posterolateral intervertebral disc herniation at the L4-L5 level with a foraminal component, L5 right-sided radiculopathy, and pronounced pain and muscle-tonic syndromes.
Upon admission, the patient complained of intense lower back pain radiating along the lateral surface of the right lower limb.
She has been suffering from this condition for several years; however, during the last month, the pain syndrome significantly worsened (9 points on the VAS). She associates the onset of the condition with the physical nature of her occupational activities.
She previously underwent conservative treatment involving physiotherapeutic procedures and sanatorium-resort therapy. However, during the last three weeks, despite the treatment, the pain in her leg intensified markedly.
Objective examination revealed pronounced tenderness upon palpation of the spinous processes of the L4 and L5 vertebrae, hypoesthesia along the L5 dermatome on the right, and a sharply positive Lasegue’s sign on the right.
MRI revealed a posterolateral intervertebral disc herniation at L4-L5 with a right-sided foraminal component and severe compression of the right L5 nerve root (Fig. 6).
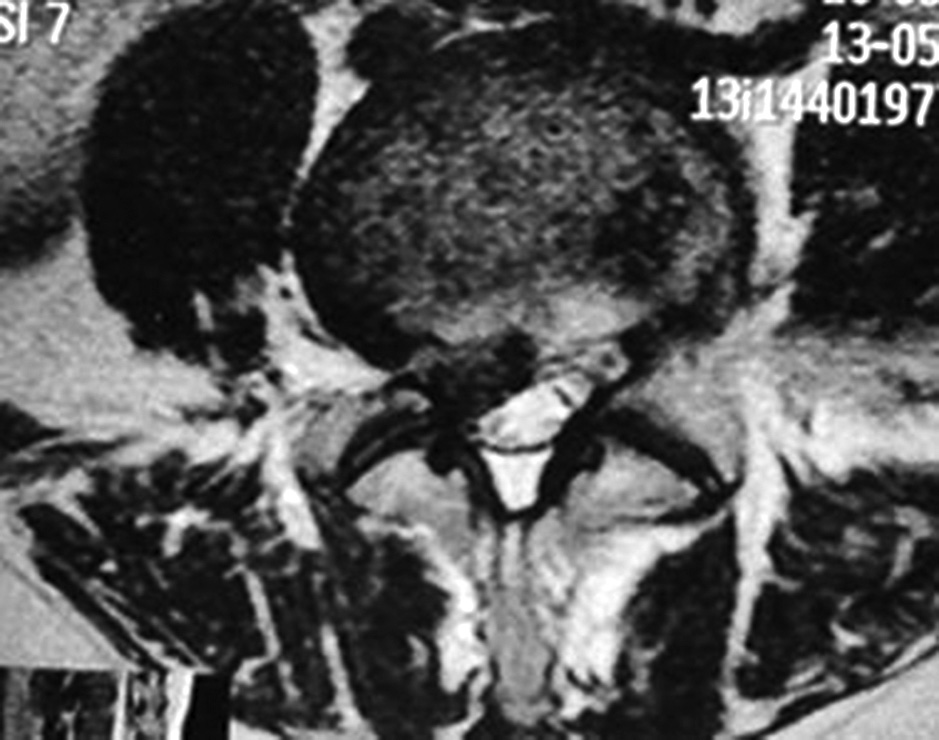
Fig. 6. MRT scan. Posterolateral herniation of the L4-L5 intervertebral disc with a right foraminal component
A transforaminal endoscopic microdiscectomy of the L4-L5 intervertebral disc on the right was performed. Fig. 7 shows fluoroscopic guidance of the endoscope port placement in the specified area of the L4-L5 intervertebral space on the right.
A B
B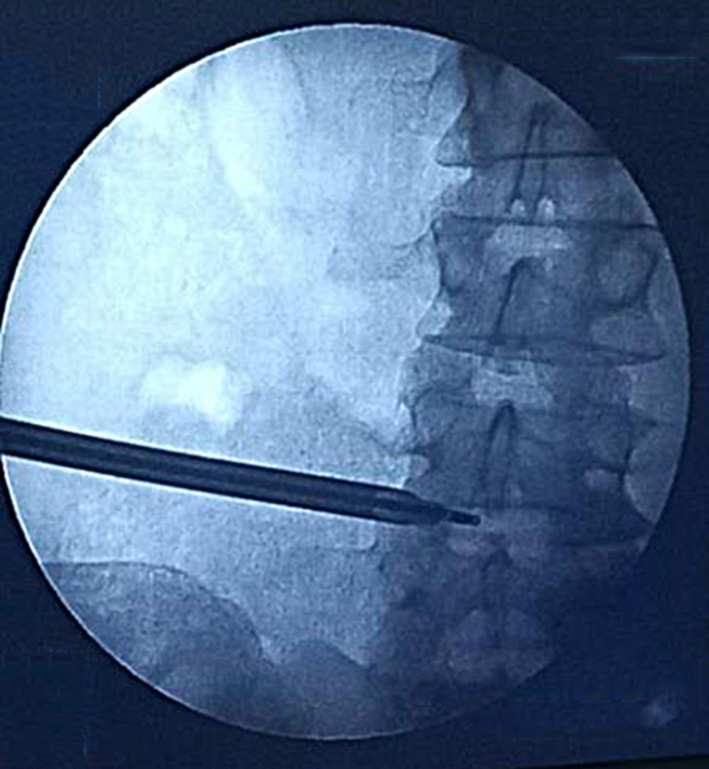
Fig. 7. Port placement: A – lateral projection; B – straight projection
Immediately after the surgery, the patient reported complete regression of the pain syndrome. She was mobilized 3 hours postoperatively. Since she resides in another city, she remained in the hospital overnight. She was discharged the following morning in satisfactory condition. Two weeks later, she reported feeling well, with no complaints and a postoperative scar showing no signs of inflammation (Fig. 8). One and a half weeks after surgery, the patient resumed her regular professional activities.

Fig. 8. Postoperative scar two weeks after surgery
Discussion
X. Tao et al. (2018) [19] conducted a randomized study assessing treatment outcomes in 462 patients (231 patients in the traditional microdiscectomy group and 231 in the endoscopic transforaminal microdiscectomy group), using the VAS and the modified J. MacNab scale at 1 day, 1 month, 3 months, and 6 months postoperatively. It was found that the TESSYS technique significantly reduces the duration of surgery, intraoperative blood loss, surgical trauma, and length of hospital stay, while accelerating rehabilitation and improving treatment outcomes. The rate of good results according to the modified J. MacNab scale was 87.88% with TESSYS and 84.85% with traditional microdiscectomy.
According to Shenghua He et al. (2018), the success rate with TESSYS reached 98% one year after surgery [20]; data from Chao Yuan et al. (2020) [21] indicate a success rate of 95%.
Future research prospects
TESSYS is a modern, highly effective, minimally invasive technique for the removal of lumbar intervertebral disc herniations. Like other surgical methods, it has its advantages and disadvantages. The primary advantage is its minimally invasive nature combined with adequate radicality when compared to traditional microdiscectomy. However, a notable disadvantage is its insufficient universality.
According to the author, future research should focus on improving the visualization of herniated discs and the planning of interventions — in particular through the use of artificial intelligence. This is especially relevant for determining the entry point, which is currently calculated in a highly subjective manner and may contribute to unsuccessful surgical outcomes. Additional research should address the "safe" placement of the endoscope port along an optimal trajectory to avoid damage to neural and vascular structures, ensure complete herniation removal, and achieve full decompression of the compressed nerve root and/or dural sac.
Conclusions
Disclosure
Conflict of interest
The author declares no conflict of interest.
Ethical standards
All procedures performed on patients during the study complied with the ethical standards of the institutional and national research ethics committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from each individual patient.
Funding
This study received no financial support or sponsorship.
References
1. Brotchi J, Pirotte B, De Witte O, Levivier M. Prevention of epidural fibrosis in a prospective series of 100 primary lumbo-sacral discectomy patients: follow-up and assessment at re-operation. Neurol Res. 1999;21 Suppl 1:S47-50. https://doi.org/10.1080/01616412.1999.11741027
2. Pedachenko EG, Tarasenko ON. [Nearest and retrospective results of patients with postoperative compressive cicatrical-adhesive epiduritis treatment]. Ukr Neurosurg J. 2006;(3):46-50. Ukrainian. https://theunj.org/article/view/127817
3. Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P 2nd, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WL Jr, Toton JF; North American Spine Society. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014 Jan;14(1):180-91. https://doi.org/10.1016/j.spinee.2013.08.003
4. Arts MP, Kuršumović A, Miller LE, Wolfs JFC, Perrin JM, Van de Kelft E, Heidecke V. Comparison of treatments for lumbar disc herniation: Systematic review with network meta-analysis. Medicine (Baltimore). 2019 Feb;98(7):e14410. https://doi.org/10.1097/MD.0000000000014410
5. Schaller B. Failed back surgery syndrome: the role of symptomatic segmental single-level instability after lumbar microdiscectomy. Eur Spine J. 2004 May;13(3):193-8. https://doi.org/10.1007/s00586-003-0632-x
6. Ramaswami R, Ghogawala Z, Weinstein JN. Management of Sciatica. N Engl J Med. 2017 Mar 23;376(12):1175-1177. https://doi.org/10.1056/NEJMclde1701008
7. Kim MJ, Lee SH, Jung ES, Son BG, Choi ES, Shin JH, Sung JK, Chi YC. Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: comparison with results of microscopic diskectomy. Surg Neurol. 2007 Dec;68(6):623-631. https://doi.org/10.1016/j.surneu.2006.12.051
8. Nellensteijn J, Ostelo R, Bartels R, Peul W, van Royen B, van Tulder M. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J. 2010 Feb;19(2):181-204. https://doi.org/10.1007/s00586-009-1155-x
9. Jasper GP, Francisco GM, Telfeian AE. A retrospective evaluation of the clinical success of transforaminal endoscopic discectomy with foraminotomy in geriatric patients. Pain Physician. 2013 May-Jun;16(3):225-9.
10. Morgenstern R. Transforaminal endoscopic stenosis surgery (TESS). The Internet Journal of Minimally Invasive Spinal Technology. 2008;3(4). https://ispub.com/IJMIST/3/4/4522
11. Hoogland T, van den Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976). 2008 Apr 20;33(9):973-8. https://doi.org/10.1097/BRS.0b013e31816c8ade
12. Zhou F, Tao H, Liu G, Zhang Y, Zhang Y, Zhou K. Clinical effect of TESSYS technique under spinal endoscopy combined with drug therapy in patients with lumbar disc herniation and its effect on quality of life and serum inflammatory factors: results of a randomized trial. Ann Palliat Med. 2021 Aug;10(8):8728-8736. https://doi.org/10.21037/apm-21-1282
13. Pan M, Li Q, Li S, Mao H, Meng B, Zhou F, Yang H. Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications. Pain Physician. 2020 Jan;23(1):49-56.
14. Pan Z, Ha Y, Yi S, Cao K. Efficacy of Transforaminal Endoscopic Spine System (TESSYS) Technique in Treating Lumbar Disc Herniation. Med Sci Monit. 2016 Feb 18;22:530-9. https://doi.org/10.12659/msm.894870
15. Ju CI, Lee SM. Complications and Management of Endoscopic Spinal Surgery. Neurospine. 2023 Mar;20(1):56-77. https://doi.org/10.14245/ns.2346226.113
16. Shi C, Wu L, Tang G, Sun B, Xu N, Lin W, Liu J, Xu G. Clinical Outcomes of Full-Endoscopic Visualized Foraminoplasty and Discectomy for Lumbar Disc Herniation with Bilateral Radiculopathy. Orthop Surg. 2024 Dec;16(12):3014-3025. https://doi.org/10.1111/os.14240
17. Chang H, Li Z, Zhang Y, Ding W, Xu J. Full-Endoscopic Foraminoplasty and Lumbar Discectomy for Single-Level Lumbar Disc Herniation. J Vis Exp. 2024 Mar 1;(205). https://doi.org/10.3791/66124
18. Xin G, Shi-Sheng H, Hai-Long Z. Morphometric analysis of the YESS and TESSYS techniques of percutaneous transforaminal endoscopic lumbar discectomy. Clin Anat. 2013 Sep;26(6):728-34. https://doi.org/10.1002/ca.22286
19. Tao XZ, Jing L, Li JH. Therapeutic effect of transforaminal endoscopic spine system in the treatment of prolapse of lumbar intervertebral disc. Eur Rev Med Pharmacol Sci. 2018 Jul;22(1 Suppl):103-110. https://doi.org/10.26355/eurrev_201807_15371
20. He S, Sun Z, Wang Y, Ma D, Tan W, Lai J. Combining YESS and TESSYS techniques during percutaneous transforaminal endoscopic discectomy for multilevel lumbar disc herniation. Medicine (Baltimore). 2018 Jul;97(28):e11240. https://doi.org/10.1097/MD.0000000000011240
21. Yuan C, Zhou Y, Pan Y, Wang J. Curative effect comparison of transforaminal endoscopic spine system and traditional open discectomy: a meta-analysis. ANZ J Surg. 2020 Jan;90(1-2):123-129. https://doi.org/10.1111/ans.15579