Original article
Ukrainian Neurosurgical Journal. 2025;31(1):34-40
https://doi.org/10.25305/unj.318715
1 Scientific and Organizational Department, Romodanov Neurosurgery Institute, Kyiv, Ukraine
2 Pain Management Center SPRAVNO, Kyiv, Ukraine
3 Department of Miniinvasive and Laser Spinal Neurosurgery, Romodanov Neurosurgery Institute, Kyiv, Ukraine
4 MedClinic Medical Center, Kyiv, Ukraine
5 Main Medical Clinical Center of the Ministry of Internal Affairs of Ukraine, Kyiv, Ukraine
Received: 23 December 2024
Accepted: 05 January 2025
Address for correspondence:
Dmytro M. Romanukha, Department of Neurosurgery, Main Medical Clinical Center of the Ministry of Internal Affairs of Ukraine, 1 Berdychivsʹka Street, Kyiv, 04116, Ukraine, e-mail: neuromanukha@gmail.com
Coccygodynia (CD) is characterized by pain in the coccyx area, but in some cases the pain radiates to the sacrum, perineum, anus, genitals, gluteal area, sacroiliac joint, lower lumbar spine and thighs. The association of СD with other pain syndromes can lead to complicated diagnosis and non-targeted treatment, which will not improve the patient's condition.
Objective: To investigate the frequency of the combination of low back pain in patients with CD who underwent spinal surgery and to evaluate the effectiveness of their treatment.
Materials and methods: An analysis of the results of 62 interventions on Ganglion Impar (GI) in 54 patients was performed. Interventions were performed in the three medical centers in Kyiv, Ukraine in the period from 2017 to 2024: Main Medical Clinical Center of the Ministry of Internal Affairs of Ukraine, Romodanov Neurosurgery Institute and MedClinic Medical Center.
Results: 14.8% of all study participants had post-traumatic CD (history of falling on the coccyx), in one case CD was caused by pelvic cancer, the vast majority of 83.3% had idiopathic CD. 21 (38.9%) of the study participants were male and 33 (61.1%) were female aged 23 to 84 years (mean age 48.015.4 years). In our series, 16 (29.6%) patients had lumbar or sciatic syndrome. Following treatment for CD, all patients noted a significant reduction of low back pain. In 4 (7.4%) observations, the intervention on GI was performed after lumbosacral spine stabilization surgery.
Conclusions: Surgical treatment of spinal pathology in patients with СD partially reduced the intensity of the pain syndrome. The execution of the GI steroid block ensured the achievement of a stable analgesic effect during the six-month follow-up. Patients presenting with CD accompanied by lumbago or radiating pain require an integrated approach to ensure accurate differential diagnosis and optimal treatment outcomes.
Key words: coccygodynia; low back pain; lumbalgia; lumbago; sciatica; pelvic pain; ganglion impar; ganglion of Walther; coccyx; spine; spinal stabilization; ganglion impar block
Introduction
Coccygodynia (CD) is pain in the coccygeal region that intensifies when sitting on hard surfaces. This pain is also provoked by leaning backward while seated. The coccyx is the terminal segment of the spine, forming a triangular bone composed of three to five fused segments (vertebrae), with the largest segment articulating with the lower sacral segment. Despite its small size, the coccyx performs several important functions: it serves as an attachment site for multiple muscles, ligaments, and tendons, and, along with the ischial tuberosities, acts as one of the "tripod" supports that bear body weight in a sitting position. Leaning backward while sitting increases pressure on the coccyx. Additionally, the coccyx plays a role in positional support of the anal region.
Idiopathic CD is the most prevalent among etiological factors [1–5]. It is believed to be associated with abnormal hypermobility of the coccygeal region—hypermobility of the coccyx and the sacrococcygeal joint—leading to chronic inflammation [1, 5, 6]. Trauma to the coccygeal area, such as from falls or childbirth, and coccygeal dislocation are the second most common causes of CD, while other etiological factors (infection, tumor, osteophyte, etc.) are significantly rarer [3, 4]. Obesity and female sex are associated with an increased risk of CD [4]. Women are more susceptible to CD due to anatomical and physiological characteristics of the pelvis, including a larger coccyx, more posterior sacral positioning, and the pressure exerted on the sacrococcygeal region during pregnancy and childbirth [7, 8].
Pain in CD may radiate to adjacent anatomical regions, including the sacrum, perineum, anus, genital organs, buttocks, sacroiliac joint, thighs, and lower lumbar spine, which can obscure the primary source of pain. This is attributed to the significant innervation of this anatomical region. On the anterior surface of the coccyx lies the ganglion impar (GI), the caudal termination of the sympathetic trunk, which provides sympathetic and nociceptive innervation to the perineum, coccyx, distal rectum, anus, distal urethra, vulva, vagina, and penis. Visceral afferents from these anatomical structures converge at the GI [9]. Postganglionic sympathetic fibers from the sympathetic trunk pass through gray communicating rami to the GI, providing sympathetic innervation to the pelvic viscera [10]. Additionally, the ventral branches of the sacral nerves pass near the GI [11].
According to the literature, CD accounts for 1–3% of cases of lower back pain, although its exact prevalence remains unknown [12]. In a study of 50 CD patients undergoing osteopathic manipulative treatment, 27 (54%) also experienced lower back pain or radicular pain syndrome [13]. The association of CD with other pain syndromes may complicate diagnosis and lead to inappropriate treatment, which does not contribute to patient recovery.
Objective: To investigate the frequency of : low back pain in patients with coccygodynia undergoing spinal surgery and to evaluate the effectiveness of their treatment.
Materials and Methods
Study Participants
A sample of patients with CD (n=54) who underwent 62 interventions on GI was analyzed. Written informed consent was obtained from all patients after a detailed explanation of the procedure.
Inclusion Criteria:
Presence of coccygeal pain for ≥3 months, patients of both sexes, age between 23 and 84 years, lack of response to analgesics, anti-inflammatory drugs, and other conservative treatment methods.
Exclusion Criteria:
Age below 16 years, presence of a local skin infection at the injection site or systemic infection,allergy to anesthetics or contrast agents, sacrococcygeal fusion due to any pathology, history of coccygectomy, coagulation profile disorders, pregnancy, psychiatric disorders, including those under psychiatric dispensary supervision, inability to continue participation in the study during the follow-up period.
Group Characteristics
Among the patients, 33 (61.1%) were female and 21 (38.9%) were male. The mean patient age was 48.0±15.4 years.
Minimally invasive GI interventions were performed using five different techniques. Ganglion impar block (GIB) was conducted in 44 patients, while alternative GI interventions were applied in cases of resistant CD following prior steroid injections. These included GI neurolysis with ethanol (n=2) or phenol (n=2), GI radiofrequency modulation (n=4), and GI radiofrequency ablation (n=10).
Study design
A prospective interventional study was conducted on the basis of three medical institutions in Kyiv, Ukraine: the Main Medical Clinical Center of the Ministry of Internal Affairs of Ukraine, the Romodanov Institute of Neurosurgery of the National Academy of Medical Sciences of Ukraine, and the «Medclinic» Medical Center, over the period from 2017 to 2024.
The study adhered to the principles of bioethics in accordance with the Declaration of Helsinki on Human Rights (1975) and its subsequent revisions (1996–2013), the Council of Europe Convention on Human Rights and Biomedicine, and the legislation of Ukraine. The study protocol was approved by the Ethics and Bioethics Committee of the Romodanov Institute of Neurosurgery, National Academy of Medical Sciences of Ukraine (Minutes No. 3, dated December 16, 2020). The study did not pose an increased risk to participants and was conducted in compliance with bioethical norms and scientific standards for clinical research involving patients.
Patient data were analyzed based on clinical assessments, including a preliminary survey using the Visual Analog Scale (VAS) for pain (0 cm – no pain, 10 cm – unbearable pain). The functional status of patients was assessed before and after the procedure using the Karnofsky Performance Scale (KPS), ranging from 0% to 100%. Patients were followed up for six months, with evaluations conducted at one week, one month, three months, and six months post-procedure.
Statistical analysis
The collected data were processed using the statistical software package MedCalc V 22.016. Quantitative variables (age, VAS, and KPS scores) were presented as mean values with standard deviations. To determine differences following the interventions, the paired Student’s t-test was used for normally distributed data, while the Wilcoxon signed-rank test was applied for non-normally distributed data. A significance level of 0.05 was considered statistically significant.
Results
Characteristics of the study material
Idiopathic CD was diagnosed in the majority of patients (83.3%) (Table 1). One female patient (1.9%) had CD due to oncological involvement of the pelvic organs and had undergone surgical intervention for this condition. Another female patient (1.9%) developed CD following the excision of a coccygeal cyst. In these cases, GIB resulted in significant pain reduction.
Table 1. Characteristics of the overall study population with coccydynia (n=54)
|
Parameter |
Number |
|
|
Abs. |
% |
|
|
Sex: |
||
|
male |
21 |
38,9 |
|
female |
33 |
61,1 |
|
Age, years |
48,0±15,4 (23‒84) |
|
|
Etiology of pain: |
||
|
idiopathic coccydynia |
45 |
83,3 |
|
trauma |
8 |
14,8 |
|
oncology |
1 |
1,9 |
In our series, 16 patients (29.6%) presented with lumbalgia or sciatic syndrome. Following treatment for CD, all patients reported significant pain relief in the lower back.
In four cases (7.4%), the intervention on the GI was performed after a stabilization surgery in the lumbosacral spine.
Clinical case analysis
Four patients (two males and two females) aged 51 to 70 years sought medical attention due to pain in the lumbosacral spine and coccyx (Tables 2 and 3). The duration of pain ranged from three months to one year. None of the patients had a history of direct coccygeal trauma. Before surgery, all patients underwent magnetic resonance imaging (MRI) of the lumbosacral spine, including the coccyx, and functional radiography of the lumbosacral spine. Based on their complaints and the findings of neurological and neuro-orthopedic examinations, surgical treatment was deemed necessary.
Table 2. Characteristics of patients with coccydynia who underwent surgical intervention on the lumbosacral spine (n=4)
|
№ |
Sex |
Age, years |
Etiology of сoccydynia |
Comorbid pathology |
Pain duration |
|
1 |
M |
51 |
Idiopathic |
LS |
6 months |
|
2 |
F |
68 |
Idiopathic |
LS HTN |
6 months |
|
3 |
M |
70 |
Idiopathic |
LS HTN |
1 year |
|
4 |
F |
54 |
Idiopathic |
LS |
3 months |
Note: *LS osteochondrosis; ** HTN - hypertension.
Table 3. Pain localization (n=4)
|
Pain localization |
||||||||||
|
|
Radicular (root) symptoms |
|||||||||
|
№ |
Coccyx |
LS spine* |
Sacrum |
SI joint** |
Perineum |
AR*** |
GO**** |
Buttock |
Thigh |
Lower leg |
|
1 |
+ |
+ |
+ |
- |
+ |
+ |
+ |
+ |
+ |
- |
|
2 |
+ |
+ |
+ |
- |
- |
- |
- |
+ |
+ |
+ |
|
3 |
+ |
+ |
+ |
- |
- |
- |
- |
+ |
+ |
+ |
|
4 |
+ |
+ |
- |
- |
- |
- |
- |
+ |
+ |
+ |
Note. *LS spine – Lumbosacral spine; **Sacroiliac joint; ***Anal region; ****Genital organs.
Prior to surgery, none of the patients exhibited a significant response to conservative pharmacological therapy or physiotherapeutic treatment methods. In three cases, transpedicular fixation of the spine was performed at the L5/S1 level, while in one case, it was conducted at the L4/L5 level. The surgical interventions were carried out without complications, and all patients were discharged in satisfactory condition, reporting a reduction in radicular pain in the lower extremities. However, the intensity of pain in the coccyx, sacrum, and lower lumbarsacral spine remained largely unchanged. The persistence of this pain syndrome, along with the presence of postoperative discomfort, hindered rapid and full recovery in patients and adversely affected their functional status. Consequently, GIB was performed, leading to a sustained reduction in pain intensity over a six-month follow-up period (Tables 4 and 5). All interventions were successfully executed on the first attempt. No difficulties arose during the procedure, and there were no cases of rectal or pelvic structure perforation. Additionally, no complications were recorded post-procedure.
Table 4. Pain syndrome intensity assessment using VAS (cm) at different follow-up periods (n=4)
|
№ |
Preoperative |
Postoperative |
Post-GI intervention |
|||
|
1 week |
1 month |
3 months |
6 months |
|||
|
1 |
8 |
8 |
3 |
2 |
1 |
2 |
|
2 |
9 |
5 |
2 |
0 |
0 |
1 |
|
3 |
9 |
7 |
1 |
1 |
2 |
2 |
|
4 |
8 |
6 |
0 |
1 |
0 |
0 |
Table 5. Functional status assessment using the KS (%) at different follow-up periods (n=4)
|
№ |
Preoperative |
Postoperative |
Post-GI intervention |
|||
|
1 week |
1 month |
3 months |
6 months |
|||
|
1 |
70 |
70 |
80 |
90 |
90 |
100 |
|
2 |
80 |
70 |
90 |
100 |
100 |
100 |
|
3 |
70 |
70 |
80 |
80 |
90 |
90 |
|
4 |
70 |
70 |
90 |
90 |
100 |
100 |
Clinical сase
Patient B., a 70-year-old male, was hospitalized with complaints of intense pain in the lumbosacral spine, radiating to the sacrococcygeal region, the right gluteal area, and the right thigh along its posterolateral surface. The pain intensity, assessed using the Visual Analog Scale (VAS), was 9 cm. Examination revealed a herniated intervertebral disc at the L4/L5 level, compressing the right L5 spinal nerve root. Functional radiography of the lumbosacral spine confirmed instability at the L4/L5 level.
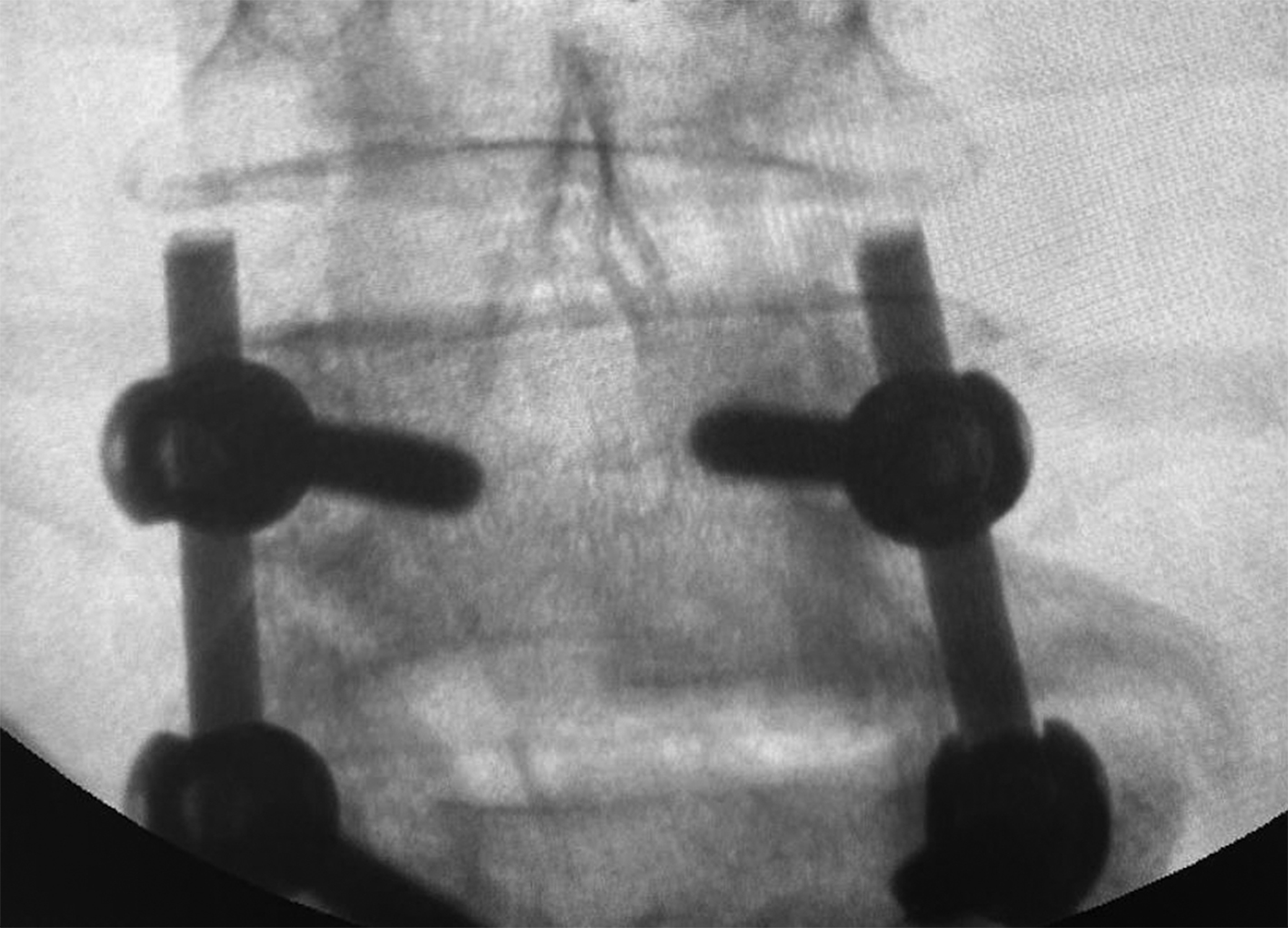
The patient underwent surgical intervention, including transpedicular fixation of the spine at the L4/L5 level and removal of the herniated intervertebral disc at L4/L5 (Fig. 1). In the postoperative period, the patient reported a reduction in pain in the right thigh; however, pain persisted in the sacrococcygeal region and the lower lumbar spine. Postoperative pain assessment using VAS was recorded at 7 cm.
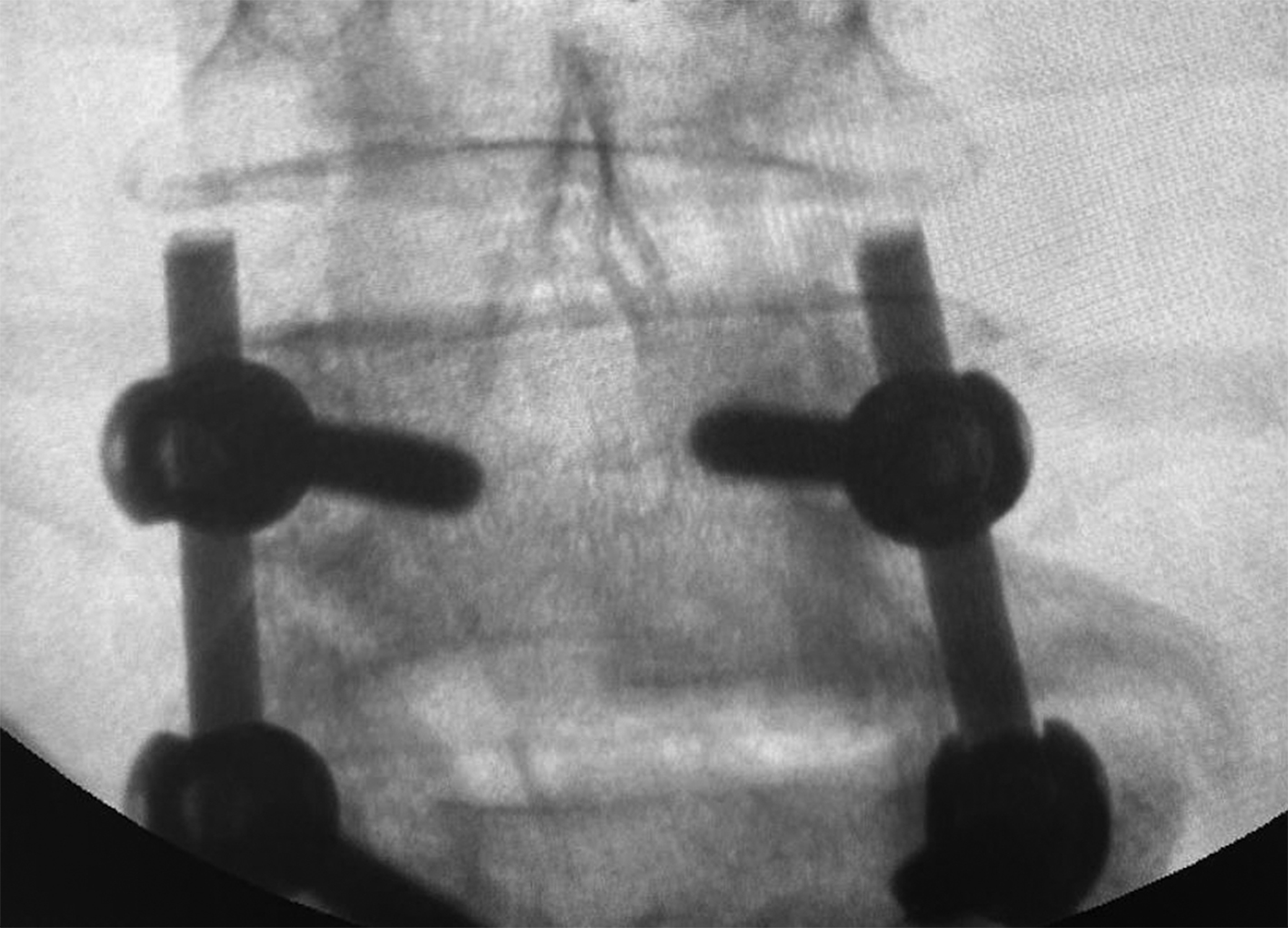
Fig. 1. Intraoperative radiographic control image of the lumbar spine in the anteroposterior view. The transpedicular fixation system is installed at the L4/L5 level
Two weeks after the surgical intervention, the patient underwent GIB using the following technique [14]. After antiseptic preparation of the skin, the target intergluteal area was covered with sterile surgical drapes. Injections were performed under fluoroscopic guidance using a C-arm. In this case, the «Cios Select with FD» device (Siemens, Germany) was used. A total of 2 mL of 2% lidocaine was administered into the subcutaneous tissue of the upper intergluteal fold as a local anesthetic, followed by the insertion of a 23G (0.6 × 30 mm) needle into the sacrococcygeal disc. The needle was advanced to the point of loss of resistance, indicating its placement anterior to the ventral sacrococcygeal ligament. Once the needle was positioned along the sacrococcygeal disc line, 1 mL of a radiopaque dye, «Tomogexol 350» (Farmak, Ukraine), diluted in saline at a 1:2–1:3 ratio, was injected. The needle position was confirmed by the appearance of a "comma" or "crescent" sign in the retroperitoneal space on lateral fluoroscopic imaging (Fig. 2). The spread of contrast within the sacrococcygeal disc indicated the need for further needle advancement. The presence of the contrast agent in the lumen of the rectum suggested posterior wall perforation and excessive needle advancement, which is an undesirable outcome. Following a negative aspiration test, confirming the absence of blood or cerebrospinal fluid, 2–3 mL of 0.5% bupivacaine and 1 mL of «Depo-Medrol®» (methylprednisolone, Pfizer, USA) were administered. One week after the GIB, the patient’s VAS score was recorded at 1 cm. The patient reported high satisfaction and was able to fully undergo the prescribed postoperative rehabilitation course.
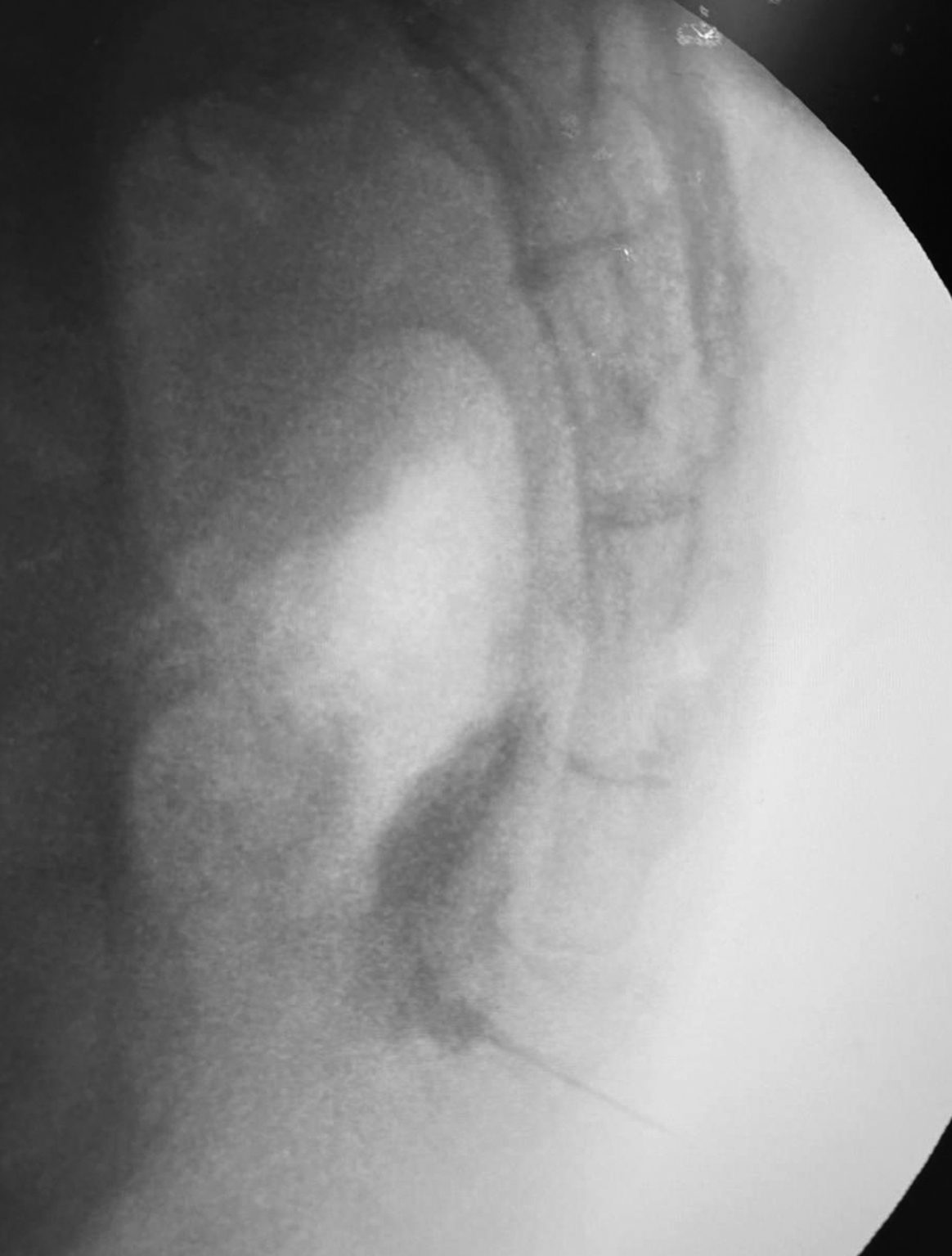
Fig. 2. GIB under X-ray control using a trans-sacrococcygeal approach, lateral projection. The needle is visualized passing through the sacrococcygeal disc, with contrast staining of the ganglion impar
Discussion
Cases of an association between low back pain and CD have been described in the literature. In the presented series of four patients with CD, two cases were accompanied by lower back pain of secondary origin due to CD. Following CD treatment with GIB, pain in both the coccyx and lower back fully regressed [5].
In another case, a 51-year-old woman sought medical attention due to lifelong persistent low back pain. Clinical examination raised suspicion of CD, and functional radiographic assessment revealed a hypermobile coccyx with dorsal angulation. The patient underwent total coccygectomy, after which the pain syndrome completely resolved, as confirmed during a follow-up examination one year postoperatively [15].
We did not find documented cases of CD occurring after similar spinal surgical interventions. Therefore, we hope this article will be valuable to the medical community. The purpose of this publication is to highlight lesser-known pain syndromes encountered in clinical practice (e.g., CD, sacroiliitis, pudendal neuralgia, Roth's syndrome) that can mimic the common presentation of low back pain.
The concepts of pain association and radiation are often conflated. However, association refers to the coexistence of different types of pain, such as the presence of multiple pain sources in a single patient (e.g., CD and lower back pain), each requiring separate treatment. In contrast, radiation describes the spread of pain from its origin (the directly affected structure or organ) to a distant location. For example, in CD, pain may radiate from the coccyx to the sacroiliac joint or the lower lumbar spine. In our series, some patients exhibited radicular symptoms triggered by degenerative spinal changes. Although surgical intervention improved their condition, complete pain regression was only observed following GIB. This suggests that the primary pain source had associated radiation, which masked the symptoms of another underlying pathology.
Currently, there are no well-defined diagnostic criteria for CD [1, 12]. Diagnosis is based on patient complaints, thorough history-taking, physical examination, and diagnostic imaging. Patients typically identify a well-localized painful area over the coccyx or report tenderness on palpation. Common symptoms include sharp coccygeal pain while sitting—especially on hard surfaces—or in a reclined position that exerts direct pressure on the coccyx. Many patients report pain when transitioning from sitting to standing, dyspareunia (pain during sexual intercourse in women), and pain during defecation. Symptoms often improve when leaning forward or shifting weight frequently between the buttocks [16].
A thorough inspection and palpation of the coccygeal region allow for the assessment of mobility, fluctuation, localized tenderness, and coccyx formation. The presence of tenderness, erythema, and swelling may indicate inflammatory processes such as cellulitis or osteomyelitis. Rash, discharge, and fistula formation may suggest a pilonidal cyst, while point tenderness at the distal tip of the coccyx may indicate degenerative osteophytes (bone spurs) [16].Rectal examination, performed by grasping the coccyx between the index finger and thumb, enables the evaluation of local sensitivity, hypomobility, and hypermobility of the sacrococcygeal joint [6]. Other potential causes of coccygeal pain include internal hemorrhoids, perineal abscesses, rectal masses, and prostate hypertrophy [17]. During a physical examination, it is essential to assess the lumbar spine for pain related to facet joint arthritis, L5-S1 intervertebral disc degeneration, and sacroiliac joint dysfunction [12]. When CD coexists with or mimics pain associated with degenerative changes in the lumbosacral spine, diagnostic challenges increase significantly.
The coccyx is not typically included in standard radiographic protocols for the lumbar spine or pelvis; therefore, the radiologist should be informed about the need to include the coccygeal region in the examination. The most critical imaging study is a lateral radiograph of the coccyx taken in both standing and seated (weight-bearing) positions [16]. The optimal protocol involves capturing standing radiographs after the patient has been upright for 5–10 minutes to ensure the coccyx is in a neutral position [18]. Seated images should be acquired while the patient is sitting on a firm surface with a slightly extended spine, applying pressure on the coccyx at an angle that provokes pain. Ideally, the patient should remain seated on a firm surface for one minute before imaging [18]. These dynamic radiographs facilitate the assessment of fractures, dislocations, hypermobility, and hypomobility. Hypermobility is defined as an inter-coccygeal angle change of >25° between sitting and standing images, while hypomobility is characterized by a change of <5° [12]. In cases where dynamic functional imaging is challenging due to pain, the recommended standing and sitting duration may be reduced. If severe or intolerable pain is present, weight-bearing projections should be avoided, and lateral projections in the supine position should be performed instead [12].
Additional radiographs, including anteroposterior and lateral views of the lumbar spine and pelvis, may be required to detect coccygeal pathology. If spondylolisthesis or other instability is observed on standard lumbar radiographs, further assessment with flexion-extension functional imaging is warranted [12].
Computed tomography (CT) of the coccyx is indicated when a fracture is suspected following direct trauma or when a more detailed evaluation of bone anatomy is needed after radiography. Magnetic resonance imaging (MRI) of the coccyx, with or without contrast, is recommended when tumors (e.g., chordoma, teratoma), abscesses, infections, or other pathological conditions are suspected [12,16]. In Ukraine, MRI of the coccyx is not mandatory when performing MRI of the lumbosacral spine; however, the coccygeal region is often included in the scan. For a more targeted assessment of pathological changes, dedicated coccygeal MRI may be prescribed.
Clinical recommendations
Conclusions
Disclosures
Conflict of Interest
The authors declare no conflicts of interest.
Ethical Standards
All procedures performed on patients in this study complied with the ethical standards of institutional and national ethics committees, as well as the 1964 Declaration of Helsinki and its subsequent amendments or equivalent ethical standards.
The study was approved by the Ethics and Bioethics Committee of the Romodanov Institute of Neurosurgery, National Academy of Medical Sciences of Ukraine (Minutes No. 3, December 16, 2020).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Funding
This study did not receive any sponsorship or financial support.
References
1. Gonnade N, Mehta N, Khera PS, Kumar D, Rajagopal R, Sharma PK. Ganglion impar block in patients with chronic coccydynia. Indian J Radiol Imaging. 2017 Jul-Sep;27(3):324-328. https://doi.org/10.4103/ijri.IJRI_294_16
2. Ghai A, Jangra P, Wadhera S, Kad N, Karwasra RK, Sahu A, Jaiswal R. A prospective study to evaluate the efficacy of ultrasound-guided ganglion impar block in patients with chronic perineal pain. Saudi J Anaesth. 2019 Apr-Jun;13(2):126-130. https://doi.org/10.4103/sja.SJA_667_18
3. Pennekamp PH, Kraft CN, Stütz A, Wallny T, Schmitt O, Diedrich O. Coccygectomy for coccygodynia: does pathogenesis matter? J Trauma. 2005 Dec;59(6):1414-9. https://doi.org/10.1097/01.ta.0000195878.50928.3c
4. Choudhary R, Kunal K, Kumar D, Nagaraju V, Verma S. Improvement in Pain Following Ganglion Impar Blocks and Radiofrequency Ablation in Coccygodynia Patients: A Systematic Review. Rev Bras Ortop (Sao Paulo). 2021 Oct 28;56(5):558-566. https://doi.org/10.1055/s-0041-1735829
5. Swain BP, Vidhya S, Kumar S. Ganglion Impar Block: A Magic Bullet to Fix Idiopathic Coccygodynia. Cureus. 2023 Jan 18;15(1):e33911. https://doi.org/10.7759/cureus.33911
6. Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J. 2014 Spring;14(1):84-7
7. Malik SH, Ahmad K, Ali L. Ganglion Impar Block For Chronic Coccydynia. J Ayub Med Coll Abbottabad. 2023 Feb-Mar;35(1):123-126. https://doi.org/10.55519/JAMC-01-11092
8. Patijn J, Janssen M, Hayek S, Mekhail N, Van Zundert J, van Kleef M. 14. Coccygodynia. Pain Pract. 2010 Nov-Dec;10(6):554-9. https://doi.org/10.1111/j.1533-2500.2010.00404.x
9. Walters A, Muhleman M, Osiro S, Bubb K, Snosek M, Shoja MM, Tubbs RS, Loukas M. One is the loneliest number: a review of the ganglion impar and its relation to pelvic pain syndromes. Clin Anat. 2013 Oct;26(7):855-61. https://doi.org/10.1002/ca.22193
10. Agarwal-Kozlowski K, Lorke DE, Habermann CR, Am Esch JS, Beck H. CT-guided blocks and neuroablation of the ganglion impar (Walther) in perineal pain: anatomy, technique, safety, and efficacy. Clin J Pain. 2009 Sep;25(7):570-6. https://doi.org/10.1097/AJP.0b013e3181a5f5c7
11. Oh CS, Chung IH, Ji HJ, Yoon DM. Clinical implications of topographic anatomy on the ganglion impar. Anesthesiology. 2004 Jul;101(1):249-50. https://doi.org/10.1097/00000542-200407000-00039
12. Gufeld L, Vossen JA, Urquia DA. Coccydynia: diagnostic and management guidance. J Nurse Pract. 2020;16:735–743. https://doi.org/10.1016/j.nurpra.2020.08.008
13. Origo D, Tarantino AG, Nonis A, Vismara L. Osteopathic manipulative treatment in chronic coccydynia: A case series. J Bodyw Mov Ther. 2018 Apr;22(2):261-265. https://doi.org/10.1016/j.jbmt.2017.06.010
14. Romanukha DM, Biloshytsky VV. Minimally Invasive Interventions on Ganglion Impar in Treatment of Patients with Coccygodynia. Ukr Neurosurg J. 2024 Mar 30(1):43-52. https://doi.org/10.25305/unj.201779
15. Benditz A, König MA. Therapieresistente Kokzygodynie sollte nicht länger als Mythos angesehen werden: Der chirurgische Zugang [Therapy-resistant coccygodynia should no longer be considered a myth: The surgical approach]. Orthopade. 2019 Jan;48(1):92-95. German. https://doi.org/10.1007/s00132-018-03665-7
16. Foye PM. Coccydynia: Tailbone Pain. Phys Med Rehabil Clin N Am. 2017 Aug;28(3):539-549. https://doi.org/10.1016/j.pmr.2017.03.006
17. Elkhashab Y, Ng A. A Review of Current Treatment Options for Coccygodynia. Curr Pain Headache Rep. 2018 Mar 19;22(4):28. https://doi.org/10.1007/s11916-018-0683-7
18. Maigne JY, Tamalet B. Standardized radiologic protocol for the study of common coccygodynia and characteristics of the lesions observed in the sitting position. Clinical elements differentiating luxation, hypermobility, and normal mobility. Spine (Phila Pa 1976). 1996 Nov 15;21(22):2588-93. https://doi.org/10.1097/00007632-199611150-00008