Review article
Ukrainian Neurosurgical Journal. 2024;30(4):3-10
https://doi.org/10.25305/unj.310374
Diakonie Klinik Mosbach, Mosbach, Germany
Received: 22 August 2024
Accepted: 04 October 2024
Address for correspondence:
Kirolos Eskandar, Neckarburkener Str. 6, 74821 Mosbach, Germany, e-mail: kiroloss.eskandar@gmail.com
Introduction: The COVID-19 pandemic, caused by SARS-CoV-2, has led to an unprecedented global health crisis. While primarily recognized for its respiratory implications, the virus has shown a significant affinity for the nervous system, resulting in a wide spectrum of neurological manifestations. This literature review explores the intersection of neurology and virology, focusing on the acute and long-term neurological effects of COVID-19.
Methods: A comprehensive review of current literature was conducted using databases such as PubMed, Scopus, and Web of Science. Relevant studies were selected based on their focus on the pathophysiology, clinical presentations, and long-term neurological outcomes of COVID-19. Special attention was given to peer-reviewed articles, meta-analyses, and clinical case reports published between 2019 and 2024.
Results: The review identifies multiple mechanisms by which SARS-CoV-2 invades the nervous system, including direct viral entry and systemic inflammation. Acute neurological manifestations include encephalitis, stroke, and Guillain-Barré syndrome, while long-term sequelae encompass cognitive impairment, neurodegeneration, and psychiatric disorders. The findings underscore the complexity of COVID-19’s impact on the nervous system, with both immediate and enduring effects.
Conclusion: Neuro-COVID represents a significant and evolving challenge in the context of the pandemic. Understanding the neurological implications of COVID-19 is crucial for improving patient outcomes and guiding future research. This review underscores the need for heightened clinical awareness and a multidisciplinary approach to effectively address the complex neuro-COVID spectrum.
Key words: Neuro-COVID; SARS-CoV-2; Neurological manifestations; Long COVID; Neuroinvasion
Introduction
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, has profoundly affected global health, leading to millions of deaths and overwhelming healthcare systems worldwide. While the respiratory symptoms of COVID-19 were initially the primary concern, it soon became apparent that the virus could affect multiple organ systems, including the nervous system. This recognition has spurred an intense focus on understanding the neurological manifestations associated with COVID-19 [1].
The global impact of COVID-19 has been unprecedented. As of 2024, the virus has led to over 770 million confirmed cases and nearly 7 million deaths worldwide. The rapid spread of SARS-CoV-2, combined with its potential for severe complications, especially in vulnerable populations, has created a significant public health challenge [2]. This global crisis has prompted extensive research into various aspects of the disease, including its neurological implications.
Viral infections have long been known to affect the nervous system. Neurotropic viruses, such as herpes simplex virus and West Nile virus, can directly invade the central nervous system (CNS), leading to conditions like encephalitis and meningitis. Other viruses can cause neurological damage indirectly through immune-mediated mechanisms or by causing systemic conditions that affect the brain, such as hypoxia or coagulopathies. SARS-CoV-2 appears to have a multifaceted impact on the nervous system, potentially through direct viral invasion, immune responses, and vascular involvement, leading to a range of neurological symptoms [3].
The rationale behind studying the neurological manifestations of COVID-19 lies in the broad spectrum of neurological symptoms reported in patients, ranging from mild headaches and anosmia to severe conditions like stroke, encephalitis, and Guillain-Barré syndrome [3]. Understanding these manifestations is crucial for improving clinical management and outcomes for patients with COVID-19. Early recognition of neurological symptoms can lead to timely interventions that may reduce morbidity and mortality associated with the disease. Furthermore, studying the mechanisms by which SARS-CoV-2 affects the nervous system could provide insights into the broader field of neurovirology, potentially leading to advances in the treatment of other viral infections that impact the nervous system [2].
Methodology:
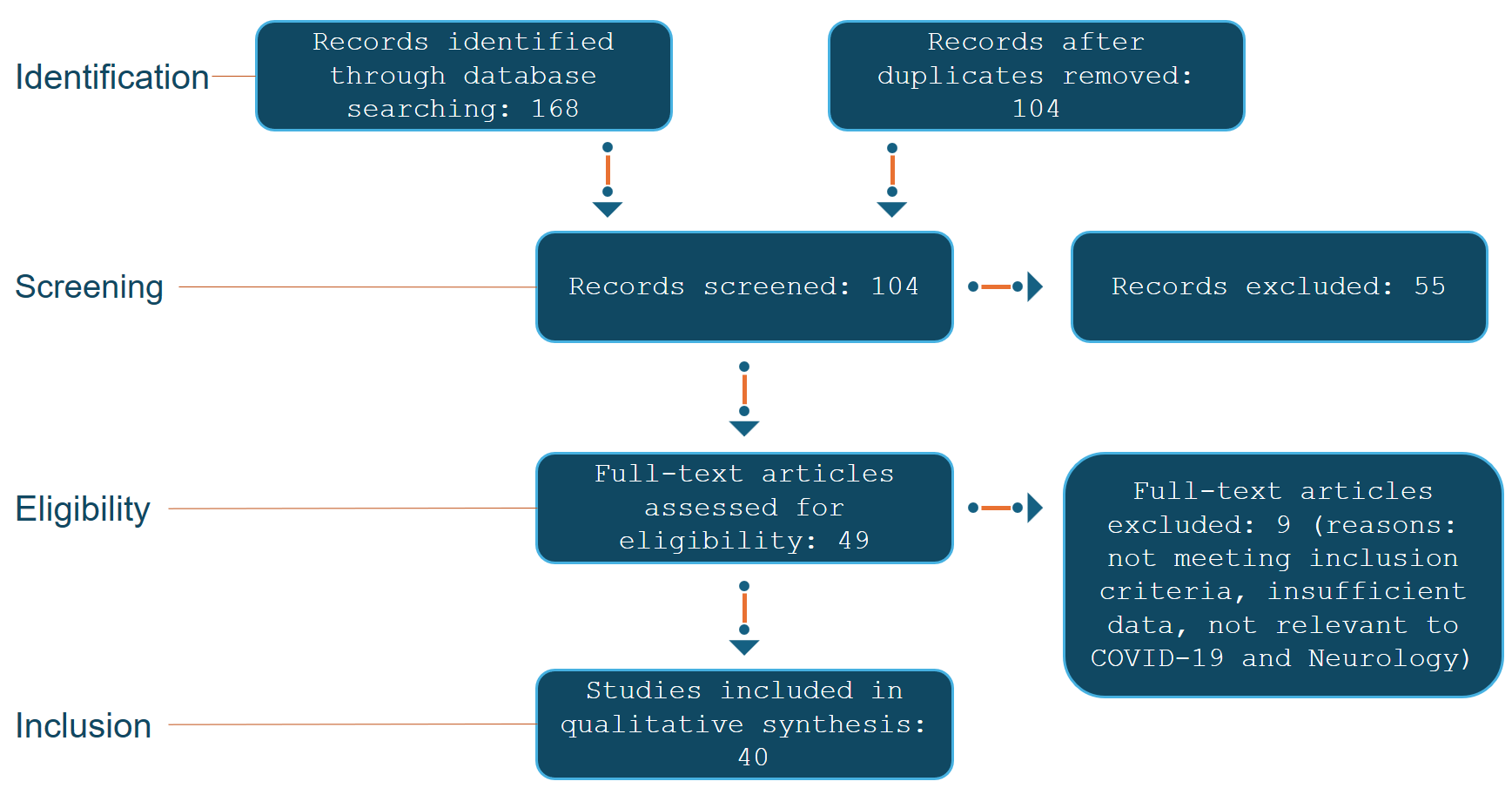
This literature review was conducted using a systematic approach in accordance with the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines to ensure a comprehensive and unbiased selection of relevant studies related to the neurological manifestations of COVID-19.
Search Strategy:
A thorough literature search was performed across several reputable databases, including PubMed, Scopus, Web of Science, and Google Scholar. The search was conducted over a period from [start date] to [end date], covering all relevant studies published during this timeframe. The search strategy incorporated a combination of specific keywords and Medical Subject Headings (MeSH) terms, including "Neuro-COVID", "SARS-CoV-2", "Neurological manifestations", "Long COVID" and "Neuroinvasion." Boolean operators (AND, OR) were used to refine the search results and ensure that a wide range of pertinent literature was captured.
Inclusion and Exclusion Criteria:
To be included in this review, studies had to meet the following criteria:
Language: Only studies published in English were considered to avoid language bias.
Population: Studies focusing specifically on patients diagnosed with COVID-19.
Focus: Articles that reported on neurological manifestations related to COVID-19.
Study Design: All types of peer-reviewed studies were included, such as case reports, cohort studies, cross-sectional studies, and reviews. Non-peer-reviewed articles, editorials, and commentaries were excluded.
Study Selection and Screening Process:
Initially, 168 articles were retrieved from the databases. After the removal of duplicate records, 120 unique articles remained. These articles were subjected to a multi-stage screening process:
Ultimately, 40 studies were included in this review after the rigorous screening process. Any discrepancies between the reviewers during the screening process were resolved through discussion or consultation with a third reviewer.
Data Extraction and Synthesis:
Data were extracted from the included studies using a standardized data extraction form. The extracted data included study characteristics (author, year, study design, sample size), patient demographics, types of neurological manifestations, and key findings related to the mechanisms and outcomes of these neurological conditions. The extracted data were then synthesized to provide a comprehensive overview of the neurological manifestations associated with COVID-19.
Quality Assessment:
The quality of the included studies was assessed using the Newcastle-Ottawa Scale for observational studies and the Cochrane Risk of Bias tool for randomized controlled trials. This assessment ensured that the findings presented in this review were based on high-quality evidence.
To provide a clear overview of the study selection process, a PRISMA flow diagram (Fig. 1) is included, illustrating the number of records identified, screened, and included in the review, along with reasons for exclusion at each stage.
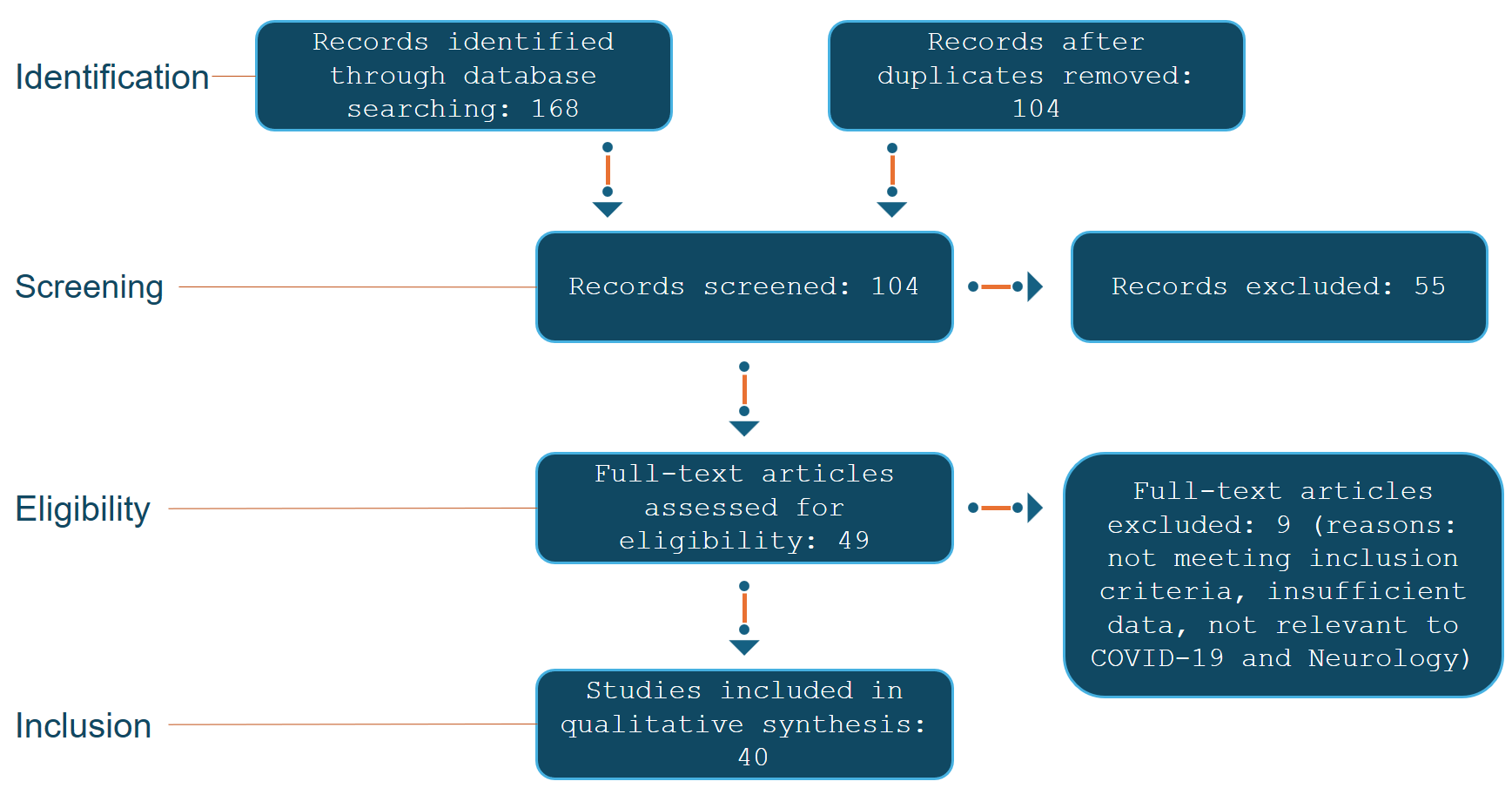
Fig. 1. Illustrates the PRIMSA flow diagram
Results:
The systematic review of the literature identified 40 studies that met the inclusion criteria and were analyzed for the neurological manifestations of COVID-19. The findings reveal a broad spectrum of both acute and long-term neurological complications associated with SARS-CoV-2 infection.
Acute Neurological Manifestations:
Central Nervous System (CNS): Encephalitis, meningitis, acute disseminated encephalomyelitis (ADEM), and ischemic stroke were frequently reported. Patients presented with symptoms ranging from mild confusion and headaches to severe cases involving coma and large-vessel strokes. Stroke, particularly in younger patients, emerged as a critical concern, with hypercoagulable states induced by the virus as a contributing factor.
Peripheral Nervous System (PNS): Guillain-Barré Syndrome (GBS) and its variants were commonly observed, presenting as ascending paralysis. Additionally, anosmia (loss of smell) and ageusia (loss of taste) were among the most prevalent early symptoms, often linked to the virus’s impact on the olfactory nerve.
Long-term Neurological Sequelae:
Cognitive and Psychiatric Disorders: Cognitive impairments, often termed "brain fog," along with headaches, fatigue, and dizziness, were recurrent in patients experiencing "Long COVID." These symptoms were compounded by mental health issues such as anxiety, depression, and PTSD.
Neurodegenerative Concerns: There is growing evidence suggesting that SARS-CoV-2 may accelerate or contribute to the onset of neurodegenerative diseases like Parkinson's and Alzheimer's. Persistent neuroinflammation and immune dysregulation are hypothesized as underlying mechanisms.
Pediatric Considerations: Conditions like Multisystem Inflammatory Syndrome in Children (MIS-C) have shown severe neurological complications, including encephalopathy and cerebrovascular events. Long-term cognitive and developmental outcomes in children who suffered from severe COVID-19 or MIS-C are still under investigation but are a significant concern.
Immunological and Molecular Insights:
The review highlighted the critical role of the immune system in the neurological impact of COVID-19, particularly the cytokine storm and its effects on the blood-brain barrier (BBB). Autoimmune responses, potentially triggered by molecular mimicry, were linked to conditions like GBS and other neuropathies, raising concerns about long-term neurodegenerative risks.
Diagnostic Challenges:
The review underscored the complexity of diagnosing COVID-19-related neurological symptoms, with neuroimaging and biomarkers like neurofilament light chain (NfL) and S100B playing crucial roles. However, the specificity of these diagnostic tools remains an area for further research.
Therapeutic Approaches:
Management strategies for these neurological manifestations have evolved, with corticosteroids like dexamethasone proving effective in reducing severe outcomes. Long-term management, particularly for "Long COVID," includes cognitive rehabilitation and neuropsychiatric support, with ongoing research into neuroprotective therapies.
Discussion:
Pathophysiology of SARS-CoV-2
The pathophysiology of SARS-CoV-2's interaction with the central nervous system (CNS) is a multifaceted process, involving both direct and indirect mechanisms of neuroinvasion. One key aspect is the virus's ability to enter the CNS, a process known as neuroinvasion. This can occur through several potential routes: direct viral entry, systemic inflammatory responses, or a combination of both.
SARS-CoV-2, like other coronaviruses, has a known neurotropic potential, which means it can infect nerve tissues. The mechanisms of neuroinvasion primarily involve two pathways: direct viral entry into the brain and the systemic inflammatory response triggered by the virus. Direct viral entry can occur through the hematogenous route, where the virus in the bloodstream crosses the blood-brain barrier (BBB) and enters the CNS. Alternatively, the virus can spread through retrograde neuronal transport, utilizing nerves like the olfactory nerve as a conduit to the brain [4].
The hematogenous spread is a critical route for neuroinvasion. After the initial infection in the respiratory system, the virus can enter the bloodstream, potentially disrupting the BBB, a protective barrier that normally restricts the entry of pathogens into the brain. SARS-CoV-2 can bind to ACE2 receptors on the endothelial cells of the BBB, leading to increased permeability and allowing the virus to penetrate the CNS. This disruption of the BBB can also result in inflammation and edema, further facilitating viral entry [5].
Another significant pathway is the olfactory route. The olfactory nerve, which extends from the nasal cavity to the brain, provides a direct route for viral entry. SARS-CoV-2 can infect the olfactory epithelial cells, which express the ACE2 receptors, and travel along the olfactory nerve into the CNS. This route of entry is particularly associated with the neurological symptom of anosmia, or loss of smell, which has been widely reported in COVID-19 patients [5, 6].
The role of the BBB in SARS-CoV-2 neuroinvasion is complex. The BBB is composed of tightly joined endothelial cells that prevent most pathogens from entering the brain. However, SARS-CoV-2 can increase the permeability of the BBB through various mechanisms, including the release of pro-inflammatory cytokines during the systemic inflammatory response known as the cytokine storm. This increased permeability allows not only the virus but also immune cells and inflammatory mediators to enter the CNS, potentially leading to neuroinflammation and neurological damage [7].
Acute Neurological Manifestations
The neurological manifestations of COVID-19 encompass a range of acute conditions involving both the central nervous system (CNS) and peripheral nervous system (PNS). Among CNS manifestations, encephalitis and meningitis are prominent, often presenting with symptoms like confusion, altered mental status, and in severe cases, coma. Acute disseminated encephalomyelitis (ADEM) has also been reported, characterized by an inflammatory attack on the brain and spinal cord, likely driven by the immune response to SARS-CoV-2 [8]. Stroke, particularly ischemic stroke, is another significant concern, with COVID-19 patients at increased risk due to hypercoagulable states induced by the virus. Reports from China and the United States have documented large-vessel strokes in younger patients, raising concerns about the broader impact of COVID-19 on cerebrovascular health [8, 9]. Seizures and status epilepticus, though less common, have been noted, particularly in severe COVID-19 cases, suggesting that SARS-CoV-2 can provoke severe neurological sequelae [10].
In the peripheral nervous system, Guillain-Barré Syndrome (GBS) and its variants, such as Miller Fisher syndrome, have been increasingly associated with COVID-19. GBS typically presents as an ascending paralysis and is thought to result from a post-infectious dysregulation of the immune system, potentially triggered by molecular mimicry between the virus and peripheral nerve components. The clinical spectrum includes acute inflammatory demyelinating polyneuropathy (AIDP) and acute motor-sensory axonal neuropathy (AMSAN), with some COVID-19 patients requiring intensive care due to respiratory failure [11, 12]. Additionally, COVID-19 has been linked to various forms of neuropathy and myopathy, with patients often experiencing muscle pain and weakness, likely due to direct viral invasion of muscle tissue or secondary to systemic inflammation [11]. Anosmia and ageusia, or the loss of smell and taste, are among the most common early symptoms, thought to result from viral invasion of the olfactory nerve or the supportive cells in the nasal epithelium, underscoring the virus's ability to affect the nervous system even in mild cases [13].
Long-term Neurological Sequelae
The long-term neurological sequelae of COVID-19, often referred to as "Long COVID," have emerged as a significant concern in the aftermath of the pandemic. These sequelae, collectively termed Post-Acute Sequelae of SARS-CoV-2 Infection (PASC), encompass a range of persistent neurological symptoms that extend beyond the acute phase of the infection. Among the most commonly reported symptoms are cognitive impairments, often referred to as "brain fog," headaches, fatigue, and dizziness [14]. Cognitive impairments can manifest as difficulties in concentration, memory, and executive function, significantly impacting daily activities and quality of life. These symptoms are believed to arise from persistent neuroinflammation and dysregulation of the immune system, as well as potential direct viral damage to the central nervous system [15].
In addition to these cognitive and sensory disturbances, Long COVID has been associated with a significant burden of mental health issues. Anxiety, depression, and post-traumatic stress disorder (PTSD) have been widely reported among survivors, exacerbating the already complex neurological landscape of Long COVID [16]. The interplay between ongoing neurological symptoms and psychological distress creates a challenging environment for both patients and healthcare providers, necessitating a multidisciplinary approach to management.
Emerging evidence also suggests that COVID-19 may accelerate or precipitate neurodegenerative processes. There is growing concern about the potential links between COVID-19 and the development of neurodegenerative diseases such as Parkinson’s disease and Alzheimer’s disease. The mechanisms underlying these associations are thought to involve chronic neuroinflammation and persistent immune activation, which could potentially contribute to the pathophysiology of these conditions [17]. Moreover, the virus’s impact on the blood-brain barrier and its potential to trigger neuroinflammatory cascades may further contribute to the risk of neurodegeneration [18].
The chronic neuroinflammatory responses triggered by COVID-19 may not only be confined to acute illness but could have lasting effects on brain health, underscoring the importance of ongoing research in this area [19]. These findings highlight the need for long-term monitoring of individuals who have recovered from COVID-19, particularly those who experience persistent neurological symptoms, to better understand the potential for long-term neurodegenerative consequences.
Immunological and Molecular Insights
The immunological and molecular mechanisms underlying the neurological complications of COVID-19 are multifaceted and complex. One of the most significant contributors to these complications is the "cytokine storm," a hyperinflammatory response triggered by the immune system's overreaction to SARS-CoV-2. This storm involves the excessive release of pro-inflammatory cytokines such as IL-6, IL-1β, and TNF-α, which can have detrimental effects on the central nervous system (CNS). The blood-brain barrier (BBB) can become compromised during this process, allowing these cytokines and other immune cells to infiltrate the CNS, leading to inflammation, neuronal damage, and a variety of neurological symptoms [20, 21].
Autoimmunity also plays a crucial role in the neurological manifestations of COVID-19. SARS-CoV-2 has been shown to induce autoimmune responses, wherein the immune system mistakenly attacks the body's own tissues, including neural tissues. This can result from molecular mimicry, where viral antigens resemble human proteins, leading to cross-reactivity. For instance, certain SARS-CoV-2 proteins have been found to share similarities with neural antigens, potentially triggering autoimmune conditions such as Guillain-Barré Syndrome (GBS) and other neuropathies [12, 22].
Molecular mimicry and cross-reactivity are particularly concerning because they suggest a mechanism by which COVID-19 could precipitate or exacerbate chronic neurological conditions. The immune response to SARS-CoV-2 might not only cause acute neurological symptoms but could also set the stage for long-term neurodegenerative diseases. The persistent immune activation and chronic inflammation observed in some COVID-19 patients could potentially contribute to the development or progression of conditions like Parkinson's disease and Alzheimer's disease [23, 24].
Pediatric Neurological Manifestations
The pediatric population has demonstrated a unique spectrum of neurological manifestations related to COVID-19, notably through conditions such as Multisystem Inflammatory Syndrome in Children (MIS-C) and Pediatric Acute-onset Neuropsychiatric Syndrome (PANS). MIS-C, a hyperinflammatory condition often triggered by SARS-CoV-2 infection, presents with a range of neurological complications including severe encephalopathy, cerebrovascular events, and acute demyelinating syndromes. These manifestations are frequently associated with systemic inflammation and may involve direct viral invasion or autoimmune mechanisms [25, 26].
PANS, which can occur after COVID-19, has been linked to neuropsychiatric symptoms like sudden onset of obsessive-compulsive disorder, tics, and other severe behavioral changes. The pathophysiology is thought to involve immune dysregulation and molecular mimicry, where the immune response against the virus cross-reacts with neural tissues, leading to neuroinflammation [26].
Moreover, there is growing concern about the long-term cognitive and developmental outcomes in children who have experienced severe COVID-19 or MIS-C. Emerging evidence suggests that these children may face persistent challenges, including cognitive deficits, memory issues, and difficulties in executive functioning, potentially due to ongoing neuroinflammation or direct neuronal injury. These long-term effects are still being studied, but they highlight the need for continued monitoring and early intervention strategies [27, 28].
Diagnostic Challenges and Biomarkers
The neurological manifestations of COVID-19 present complex diagnostic challenges, necessitating a multifaceted approach involving advanced neuroimaging techniques and biomarkers to differentiate these symptoms from other neurological disorders. Neuroimaging, including MRI, CT, and PET scans, plays a critical role in identifying the structural and functional alterations in the brain associated with COVID-19. MRI has been particularly useful in detecting white matter hyperintensities, microhemorrhages, and cortical abnormalities, which are indicative of the neuroinflammatory processes triggered by SARS-CoV-2 infection. PET scans, although less frequently utilized, have shown changes in glucose metabolism, especially in the frontal and temporal lobes, correlating with cognitive deficits like "brain fog" commonly reported in long COVID cases [28].
Cerebrospinal fluid (CSF) analysis offers another diagnostic avenue, providing insights into the immune response and neuronal injury associated with COVID-19. Elevated levels of neurofilament light chain (NfL) in the CSF have been correlated with neuronal damage, and this marker has been proposed as a potential biomarker for assessing the severity of neurological involvement in COVID-19. Additionally, the presence of oligoclonal bands (OCBs) in the CSF has been linked to intrathecal antibody synthesis, suggesting an ongoing immune response within the central nervous system [29].
Differential diagnosis remains a critical challenge, as many of the neurological symptoms of COVID-19 overlap with other conditions, such as autoimmune encephalitis, stroke, and neurodegenerative diseases. Biomarkers like NfL and S100B, combined with neuroimaging findings, are essential for distinguishing COVID-19-related neurological damage from other etiologies [30]. However, the specificity and sensitivity of these biomarkers are still under investigation, and further research is needed to refine their diagnostic utility [31].
Therapeutic Approaches and Management
The therapeutic management of neurological complications associated with COVID-19 encompasses a broad range of strategies tailored to address both acute and long-term effects. The complexity of these neurological manifestations requires a multidisciplinary approach that combines pharmacological interventions, rehabilitation programs, and ongoing research into neuroprotective and anti-inflammatory therapies.
In the acute phase of COVID-19, early recognition and treatment of neurological complications are critical. Corticosteroids, particularly dexamethasone, have demonstrated significant efficacy in reducing inflammation and preventing severe neurological outcomes such as stroke, encephalitis, and seizures. Dexamethasone works by dampening the hyperinflammatory response associated with severe COVID-19, which is a key contributor to the development of neurological complications. Additionally, antiviral agents like remdesivir, when used in conjunction with corticosteroids, have been shown to synergistically reduce the frequency and severity of neurological manifestations, thereby improving overall patient outcomes [32].
As the pandemic has progressed, the focus has increasingly shifted towards managing the long-term neurological sequelae of COVID-19, commonly referred to as "long COVID" or post-acute sequelae of SARS-CoV-2 infection (PASC). These long-term symptoms include cognitive impairments such as "brain fog," chronic headaches, fatigue, and neuropsychiatric disorders like anxiety, depression, and post-traumatic stress disorder (PTSD). Cognitive rehabilitation, which includes strategies to enhance memory, attention, and executive function, has become a cornerstone of management for these patients. Furthermore, neuropsychiatric rehabilitation, including psychotherapy and pharmacotherapy, is crucial for addressing the mental health challenges associated with long COVID [33].
Research into neuroprotective agents is ongoing, with a focus on their potential to prevent or mitigate long-term neurodegenerative processes that may be initiated by COVID-19. Agents such as N-acetylcysteine (NAC) and melatonin are being investigated for their antioxidant properties and their ability to reduce oxidative stress and inflammation in the brain. These agents could play a role in protecting neuronal integrity and preventing the progression of neurodegenerative diseases in patients with a history of COVID-19 [34].
Given the central role of inflammation in COVID-19-related neurological damage, anti-inflammatory therapies are a key area of interest. Beyond corticosteroids, other anti-inflammatory agents, including interleukin-6 (IL-6) inhibitors (e.g., tocilizumab) and Janus kinase (JAK) inhibitors, are being explored for their potential to modulate the immune response and reduce neuroinflammation. These therapies aim to target the chronic inflammatory state that persists in some patients post-COVID-19, which is thought to contribute to the development of long-term neurological complications [35].
Rehabilitation plays an essential role in the recovery of patients with neurological complications from COVID-19. Multidisciplinary rehabilitation programs that incorporate physical therapy, occupational therapy, speech therapy, and neuropsychological support are vital for helping patients regain function and improve their quality of life. Telemedicine has also emerged as a valuable tool in delivering rehabilitation services to patients with long COVID, providing access to care while minimizing the risk of infection [36].
Future Directions and Research Gaps
The neurological impact of COVID-19 has revealed several critical gaps in our understanding, necessitating focused future research. A primary area of concern is the lack of comprehensive longitudinal studies that can track the neurological effects of COVID-19 over time. These studies are essential to discern the long-term consequences, particularly the risk of developing chronic neurodegenerative conditions like Alzheimer's or Parkinson's disease. Current evidence suggests that SARS-CoV-2 may accelerate neurodegenerative processes, but definitive conclusions can only be drawn through extensive follow-up research over many years [37, 38].
In parallel, there is a growing interest in developing targeted therapies for neuro-COVID. These include anti-inflammatory treatments to mitigate neuroinflammation, which has been implicated in both acute and long-term neurological symptoms of COVID-19. Researchers are also exploring the potential of neuroprotective agents that could safeguard against the neuronal damage observed in severe cases. Importantly, there is an emerging need to personalize these therapies based on individual patient profiles, taking into account factors such as genetic predispositions and the severity of initial COVID-19 infection [39].
Ethical considerations are paramount in this ongoing research. The urgency to develop treatments must be balanced with the need for thorough testing to avoid unintended consequences. Furthermore, addressing neuro-COVID requires a multidisciplinary approach, involving neurologists, immunologists, psychologists, and other healthcare professionals. This collaboration is crucial to ensure that all aspects of the condition are understood and effectively managed [40].
Conclusion
In conclusion, this review highlights the profound and multifaceted neurological impact of COVID-19, ranging from acute manifestations such as encephalitis and stroke to long-term sequelae like cognitive impairment and neurodegeneration. The pathophysiology of SARS-CoV-2’s neuroinvasion involves complex mechanisms including direct viral entry, systemic inflammation, and disruption of the blood-brain barrier. Emerging therapeutic strategies are being developed to address these neurological complications, though the field still faces significant challenges. Future research must focus on longitudinal studies to fully understand the chronic effects of COVID-19 on the nervous system, and interdisciplinary collaboration will be crucial in developing effective treatments and addressing the ethical considerations inherent in this rapidly evolving area of study.
Disclosure
Ethics approval and consent to participate:
Not applicable
Consent for publication:
Not applicable
Availability of data and material:
Data sharing not applicable to this article as no data-sets were generated or analyzed during the current study
Competing interests:
The authors declare that they have no competing interests.
Funding:
Not applicable
Acknowledgements:
Not applicable
References
1. Yu H, Sun T, Feng J. Complications and Pathophysiology of COVID-19 in the Nervous System. Front Neurol. 2020 Dec 4;11:573421. https://doi.org/10.3389/fneur.2020.5734216
2. Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger KA, Skliut M, Weinberger J, Dangayach NS, Bederson JB, Tuhrim S, Fifi JT. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N Engl J Med. 2020 May 14;382(20):e60. https://doi.org/10.1056/NEJMc20097874
3. Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, Sultan M, Easton A, Breen G, Zandi M, Coles JP, Manji H, Al-Shahi Salman R, Menon DK, Nicholson TR, Benjamin LA, Carson A, Smith C, Turner MR, Solomon T, Kneen R, Pett SL, Galea I, Thomas RH, Michael BD; CoroNerve Study Group. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020 Oct;7(10):875-882. https://doi.org/10.1016/S2215-0366(20)30287-X
4. Meinhardt J, Radke J, Dittmayer C, Franz J, Thomas C, Mothes R, Laue M, Schneider J, Brünink S, Greuel S, Lehmann M, Hassan O, Aschman T, Schumann E, Chua RL, Conrad C, Eils R, Stenzel W, Windgassen M, Rößler L, Goebel HH, Gelderblom HR, Martin H, Nitsche A, Schulz-Schaeffer WJ, Hakroush S, Winkler MS, Tampe B, Scheibe F, Körtvélyessy P, Reinhold D, Siegmund B, Kühl AA, Elezkurtaj S, Horst D, Oesterhelweg L, Tsokos M, Ingold-Heppner B, Stadelmann C, Drosten C, Corman VM, Radbruch H, Heppner FL. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci. 2021 Feb;24(2):168-175. https://doi.org/10.1038/s41593-020-00758-5
5. Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, Sordillo EM, Fowkes M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol. 2020 Jul;92(7):699-702. https://doi.org/10.1002/jmv.259150
6. Kabbani N, Olds JL. Does COVID19 Infect the Brain? If So, Smokers Might Be at a Higher Risk. Mol Pharmacol. 2020 May;97(5):351-353. https://doi.org/10.1124/molpharm.120.0000148
7. Nath A. Neurologic complications of coronavirus infections. Neurology. 2020 May 12;94(19):809-810. https://doi.org/10.1212/WNL.0000000000009455
8. Baig AM. Chronic COVID syndrome: Need for an appropriate medical terminology for long-COVID and COVID long-haulers. J Med Virol. 2021 May;93(5):2555-2556. https://doi.org/10.1002/jmv.26624
9. Li Y, Li M, Wang M, Zhou Y, Chang J, Xian Y, Wang D, Mao L, Jin H, Hu B. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol. 2020 Sep;5(3):279-284. https://doi.org/10.1136/svn-2020-0004314
10. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020 Jun 1;77(6):683-690. https://doi.org/10.1001/jamaneurol.2020.11278
11. Paterson RW, Brown RL, Benjamin L, Nortley R, Wiethoff S, Bharucha T, Jayaseelan DL, Kumar G, Raftopoulos RE, Zambreanu L, Vivekanandam V, Khoo A, Geraldes R, Chinthapalli K, Boyd E, Tuzlali H, Price G, Christofi G, Morrow J, McNamara P, McLoughlin B, Lim ST, Mehta PR, Levee V, Keddie S, Yong W, Trip SA, Foulkes AJM, Hotton G, Miller TD, Everitt AD, Carswell C, Davies NWS, Yoong M, Attwell D, Sreedharan J, Silber E, Schott JM, Chandratheva A, Perry RJ, Simister R, Checkley A, Longley N, Farmer SF, Carletti F, Houlihan C, Thom M, Lunn MP, Spillane J, Howard R, Vincent A, Werring DJ, Hoskote C, Jäger HR, Manji H, Zandi MS. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020 Oct 1;143(10):3104-3120. https://doi.org/10.1093/brain/awaa2407
12. Caress JB, Castoro RJ, Simmons Z, Scelsa SN, Lewis RA, Ahlawat A, Narayanaswami P. COVID-19-associated Guillain-Barré syndrome: The early pandemic experience. Muscle Nerve. 2020 Oct;62(4):485-491. https://doi.org/10.1002/mus.270240
13. Keddie S, Pakpoor J, Mousele C, Pipis M, Machado PM, Foster M, Record CJ, Keh RYS, Fehmi J, Paterson RW, Bharambe V, Clayton LM, Allen C, Price O, Wall J, Kiss-Csenki A, Rathnasabapathi DP, Geraldes R, Yermakova T, King-Robson J, Zosmer M, Rajakulendran S, Sumaria S, Farmer SF, Nortley R, Marshall CR, Newman EJ, Nirmalananthan N, Kumar G, Pinto AA, Holt J, Lavin TM, Brennan KM, Zandi MS, Jayaseelan DL, Pritchard J, Hadden RDM, Manji H, Willison HJ, Rinaldi S, Carr AS, Lunn MP. Epidemiological and cohort study finds no association between COVID-19 and Guillain-Barré syndrome. Brain. 2021 Mar 3;144(2):682-693. https://doi.org/10.1093/brain/awaa4339
14. Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L, Rusconi S, Gervasoni C, Ridolfo AL, Rizzardini G, Antinori S, Galli M. Self-reported Olfactory and Taste Disorders in Patients With Severe Acute Respiratory Coronavirus 2 Infection: A Cross-sectional Study. Clin Infect Dis. 2020 Jul 28;71(15):889-890. https://doi.org/10.1093/cid/ciaa3308
15. NIH study identifies features of Long COVID neurological symptoms. National Institutes of Health (NIH). 2023, May 5. https://www.nih.gov/news-events/news-releases/nih-study-identifies-features-long-covid-neurological-symptoms#:~:text=People%20with%20post%2Dacute%20sequelae,SARS%2DCoV%2D2%20infection
16. Zubair AS, McAlpine LS, Gardin T, Farhadian S, Kuruvilla DE, Spudich S. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol. 2020 Aug 1;77(8):1018-1027. https://doi.org/10.1001/jamaneurol.2020.20657
17. Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, Pujol JC, Klaser K, Antonelli M, Canas LS, Molteni E, Modat M, Jorge Cardoso M, May A, Ganesh S, Davies R, Nguyen LH, Drew DA, Astley CM, Joshi AD, Merino J, Tsereteli N, Fall T, Gomez MF, Duncan EL, Menni C, Williams FMK, Franks PW, Chan AT, Wolf J, Ourselin S, Spector T, Steves CJ. Attributes and predictors of long COVID. Nat Med. 2021 Apr;27(4):626-631. https://doi.org/10.1038/s41591-021-01292-y
18. Heneka MT, Golenbock D, Latz E, Morgan D, Brown R. Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimers Res Ther. 2020 Jun 4;12(1):69. https://doi.org/10.1186/s13195-020-00640-31
19. Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021 May;8(5):416-427. https://doi.org/10.1016/S2215-0366(21)00084-58
20. Holder K, Reddy PH. The COVID-19 Effect on the Immune System and Mitochondrial Dynamics in Diabetes, Obesity, and Dementia. Neuroscientist. 2021 Aug;27(4):331-339. https://doi.org/10.1177/1073858420960443
21. Schreiner P, Harrer T, Scheibenbogen C, Lamer S, Schlosser A, Naviaux RK, Prusty BK. Human Herpesvirus-6 Reactivation, Mitochondrial Fragmentation, and the Coordination of Antiviral and Metabolic Phenotypes in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Immunohorizons. 2020 Apr 23;4(4):201-215. https://doi.org/10.4049/immunohorizons.2000006
22. Roep BO. Molecular mimicry in autoimmune neurological disease after viral infection. Curr Med Chem. 2003 Oct;10(19):1939-43.
23. Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem Neurosci. 2020 Apr 1;11(7):995-998. https://doi.org/10.1021/acschemneuro.0c00122
24. Wang Y, Liu S, Liu H, Li W, Lin F, Jiang L, Li X, Xu P, Zhang L, Zhao L, Cao Y, Kang J, Yang J, Li L, Liu X, Li Y, Nie R, Mu J, Lu F, Zhao S, Lu J, Zhao J. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol. 2020 Oct;73(4):807-816. https://doi.org/10.1016/j.jhep.2020.05.0020
25. Santos MO, Gonçalves LC, Silva PAN, Moreira ALE, Ito CRM, Peixoto FAO, Wastowski IJ, Carneiro LC, Avelino MAG. Multisystem inflammatory syndrome (MIS-C): a systematic review and meta-analysis of clinical characteristics, treatment, and outcomes. J Pediatr (Rio J). 2022 Jul-Aug;98(4):338-349. https://doi.org/10.1016/j.jped.2021.08.0061
26. LaRovere KL, Riggs BJ, Poussaint TY, Young CC, Newhams MM, Maamari M, Walker TC, Singh AR, Dapul H, Hobbs CV, McLaughlin GE, Son MBF, Maddux AB, Clouser KN, Rowan CM, McGuire JK, Fitzgerald JC, Gertz SJ, Shein SL, Munoz AC, Thomas NJ, Irby K, Levy ER, Staat MA, Tenforde MW, Feldstein LR, Halasa NB, Giuliano JS Jr, Hall MW, Kong M, Carroll CL, Schuster JE, Doymaz S, Loftis LL, Tarquinio KM, Babbitt CJ, Nofziger RA, Kleinman LC, Keenaghan MA, Cvijanovich NZ, Spinella PC, Hume JR, Wellnitz K, Mack EH, Michelson KN, Flori HR, Patel MM, Randolph AG; Overcoming COVID-19 Investigators. Neurologic Involvement in Children and Adolescents Hospitalized in the United States for COVID-19 or Multisystem Inflammatory Syndrome. JAMA Neurol. 2021 May 1;78(5):536-547. https://doi.org/10.1001/jamaneurol.2021.05049
27. Morand, A.; Urbina, D.; Fabre, A. COVID-19 and Kawasaki Like Disease: The Known-Known, the Unknown-Known and the Unknown-Unknown. Preprints 2020, 2020050160. https://doi.org/10.20944/preprints202005.0160.v1
28. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, Cook JR, Nordvig AS, Shalev D, Sehrawat TS, Ahluwalia N, Bikdeli B, Dietz D, Der-Nigoghossian C, Liyanage-Don N, Rosner GF, Bernstein EJ, Mohan S, Beckley AA, Seres DS, Choueiri TK, Uriel N, Ausiello JC, Accili D, Freedberg DE, Baldwin M, Schwartz A, Brodie D, Garcia CK, Elkind MSV, Connors JM, Bilezikian JP, Landry DW, Wan EY. Post-acute COVID-19 syndrome. Nat Med. 2021 Apr;27(4):601-615. https://doi.org/10.1038/s41591-021-01283-z7
29. Avittan H, Kustovs D. Cognition and Mental Health in Pediatric Patients Following COVID-19. Int J Environ Res Public Health. 2023 Mar 13;20(6):5061. https://doi.org/10.3390/ijerph200650618
30. Sharma VK, Singh TG, Mehta V, Mannan A. Biomarkers: Role and Scope in Neurological Disorders. Neurochem Res. 2023 Jul;48(7):2029-2058. https://doi.org/10.1007/s11064-023-03873-4
31. Kanberg N, Simrén J, Edén A, Andersson LM, Nilsson S, Ashton NJ, Sundvall PD, Nellgård B, Blennow K, Zetterberg H, Gisslén M. Neurochemical signs of astrocytic and neuronal injury in acute COVID-19 normalizes during long-term follow-up. EBioMedicine. 2021 Aug;70:103512. https://doi.org/10.1016/j.ebiom.2021.1035128
32. Paterson RW, Benjamin LA, Mehta PR, Brown RL, Athauda D, Ashton NJ, Leckey CA, Ziff OJ, Heaney J, Heslegrave AJ, Benedet AL, Blennow K, Checkley AM, Houlihan CF, Mummery CJ, Lunn MP, Manji H, Zandi MS, Keddie S, Chou M, Vinayan Changaradil D, Solomon T, Keshavan A, Barker S, Jäger HR, Carletti F, Simister R, Werring DJ, Spyer MJ, Nastouli E, Gauthier S, Rosa-Neto P; UCLH Queen Square COVID-19 Biomarker Study Group; Zetterberg H, Schott JM. Serum and cerebrospinal fluid biomarker profiles in acute SARS-CoV-2-associated neurological syndromes. Brain Commun. 2021 May 12;3(3):fcab099. https://doi.org/10.1093/braincomms/fcab0999
33. Barbosa-Silva MC, Lima MN, Battaglini D, Robba C, Pelosi P, Rocco PRM, Maron-Gutierrez T. Infectious disease-associated encephalopathies. Crit Care. 2021 Jul 6;25(1):236. https://doi.org/10.1186/s13054-021-03659-65
34. Kiani L. Preventing COVID-19 neurological complications. Nat Rev Neurol. 2022 Dec;18(12):699. https://doi.org/10.1038/s41582-022-00744-42
35. Rolin S, Chakales A, Verduzco-Gutierrez M. Rehabilitation Strategies for Cognitive and Neuropsychiatric Manifestations of COVID-19. Curr Phys Med Rehabil Rep. 2022;10(3):182-187. https://doi.org/10.1007/s40141-022-00352-97
36. Fotuhi M, Mian A, Meysami S, Raji CA. Neurobiology of COVID-19. J Alzheimers Dis. 2020;76(1):3-19. https://doi.org/10.3233/JAD-2005817
37. Thankachen SS, Devasenapathy N, Bassi A, Ghosh A, Arfin S, Gummidi B, Basheer A, Bangi A, Sahu D, Bhalla A, Blesson M, Jain M, Jha V. Colchicine to reduce coronavirus disease-19-related inflammation and cardiovascular complications in high-risk patients post-acute infection with SARS-COV-2-a study protocol for a randomized controlled trial. Trials. 2024 Jun 12;25(1):378. https://doi.org/10.1186/s13063-024-08205-76
38. Daniels K, Mourad J, Bonnechère B. Exploring the Use of Mobile Health for the Rehabilitation of Long COVID Patients: A Scoping Review. Healthcare (Basel). 2024 Feb 10;12(4):451. https://doi.org/10.3390/healthcare120404516
39. D'Arcy RCN, Sandhu JK, Marshall S, Besemann M. Mitigating Long-Term COVID-19 Consequences on Brain Health. Front Neurol. 2021 Sep 27;12:630986. https://doi.org/10.3389/fneur.2021.6309864
40. Frank MG, Ball JB, Hopkins S, Kelley T, Kuzma AJ, Thompson RS, Fleshner M, Maier SF. SARS-CoV-2 S1 subunit produces a protracted priming of the neuroinflammatory, physiological, and behavioral responses to a remote immune challenge: A role for corticosteroids. Brain Behav Immun. 2024 Oct;121:87-103. https://doi.org/10.1016/j.bbi.2024.07.034