 B
B 
Case Report
Ukrainian Neurosurgical Journal. 2024;30(3):52-55
https://doi.org/10.25305/unj.306743
Ajay Sebastian Carvalho 1, Vijay Kumar Gupta 2, Chinmaya Srivatsava 1, Deepak Dwivedi 3
1 Department of Neurosurgery, Command Hospital Eastern Command, Kolkata, India
2 Department of Neurosurgery, National Institute of Medical Sciences and Research (NIMS), Jaipur, Rajasthan, India
3 Department of Anaesthesia and Critical Care, Command Hospital Eastern Command, Kolkata, India
Received: 23 June 2024
Accepted: 31 July 2024
Address for correspondence:
Ajay Sebastian Carvalho, Department of Neurosurgery, Command Hospital Eastern Command, 17/1E, Alipore Rd, Alipore Police Line, Alipore, Kolkata, West Bengal 700027, India, e-mail:ajayneuro0404@gmail.com
A case of meningocele manqué with its management is presented and the literature of this rarely reported condition is reviewed.
A one-year-old child was admitted with a small sac like lesion in the upper dorsal region with a soft swelling in the dorso lumbar region, was also associated with congenital bilateral talipes equinovarus which was being treated by a paediatric orthopedic surgeon.
Methods. Craniospinal MRI was suggestive of dorso lumbar lipomyelomeningocele, and corresponding to the dorsal sinus/sac at DV3/DV4 level there was another tethering seen on the MRI due to a band and associated with syrinx of the dorsal cord below that, s/o meningocele manqué.
Treatment. This patient underwent in 1st stage, DV2 to DV5 laminoplasty, excision of the sinus, durotomy, dissection of the multiple arachnoid cysts, and cutting of the dorsal band. In second stage will undergo surgery for Lipomyelomeningocele
Conclusion: Meningocele Manque is rare, it can present in isolation or associated with other spinal dysraphism. With other spinal dysraphism they can be either at the same or at another location, as was seen in our case. Before operating all cases of spinal dysraphism it is of paramount importance to MRI screen the entire neuraxis and study images thoroughly. In our case along with the dorso lumbar lipomyelomeningocele, there was a Meningocele manqué at DV3/DV4 level. It is essential that the meningocele manqué be addressed first; if not the returning/recoiling cord after de-tethering at the lower level can get tugged/sheared at the tethered meningocele manqué causing deficits.
Key words: meningocele manqué; spinal dysraphism; tethered cord; lipomyelomeningocele
Introduction
Meningocele Manque is a rare anomaly and is also rarely reported. It can present in isolation or with other spinal dysraphism. With other spinal dysraphism they can be either at the same or, as was in our case at another location. Before operating all cases of spinal dysraphism it is of paramount importance to MRI screen the entire neuraxis and study images thoroughly. In our case along with the dorso lumbar lipomyelomeningocele, there was a Meningocele manqué at the DV3/DV4 level. It is essential that the meningocele manqué is detected in all spinal dysraphism and addressed first; if not the returning/recoiling cord, after de-tethering at the lower level can get tugged/sheared at the tethered meningocele manqué causing deficits.
Clinical profile
One year old male child, first born of non-consanguineous marriage, a known case of Talipes equinovarus (TEV) on regular Paediatric Orthopedic consultation, was presented to paediatric OPD with the parents giving history of a soft swelling on the lower back region and a small sac like lesion on the upper back, they also reported history of reduced movements of the left lower limb as compared to the right lower limb. Urine stream was good. There were no associated delayed milestones. On examination there was a small sac like lesion (atretic meningocele) at DV3/DV4 level in the dorsal spine (Fig. 1A), lipomyelomeningocele in the dorso lumbar region (Fig. 1B) and TEV, there were no other cutaneous stigmata, neurologically the power in left lower limb was less as compared to right.
A  B
B 
Fig. 1. A - showing the dormant sinus/sac upper dorsal level (green arrow), B –showing the lipoma (part of lipomyelomeningocele) (blue arrow)
MRI of entire neuraxis revealed a lipomyelomeningocele (Fig. 2) with associated low lying cord with tethering. However at DV3/DV4 level corresponding to the dorsal sinus/sac there was another tethering of the dorsal cord due to a fibrous band associated with syrinx (Fig. 3), there was no associated Chiari malformation.
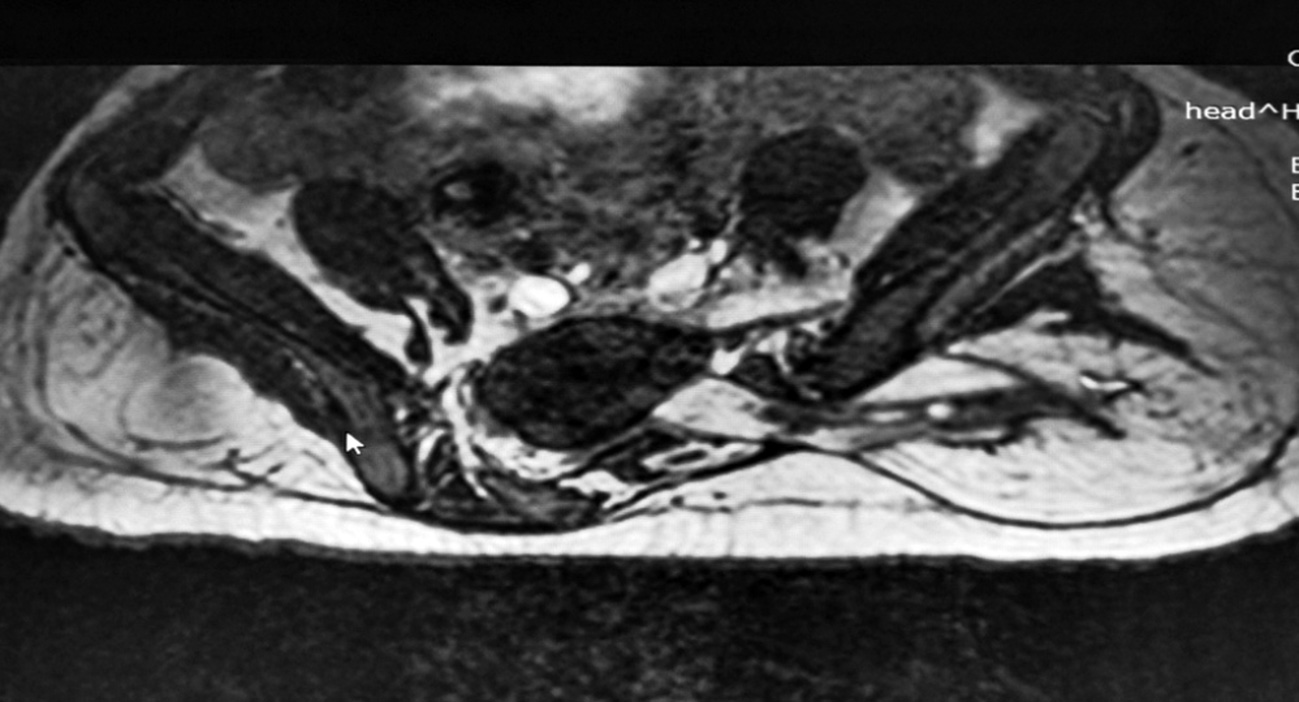
Fig. 2. Representative T2W axial cuts of the Lumbosacral spine showing the lipomyelomeningocele
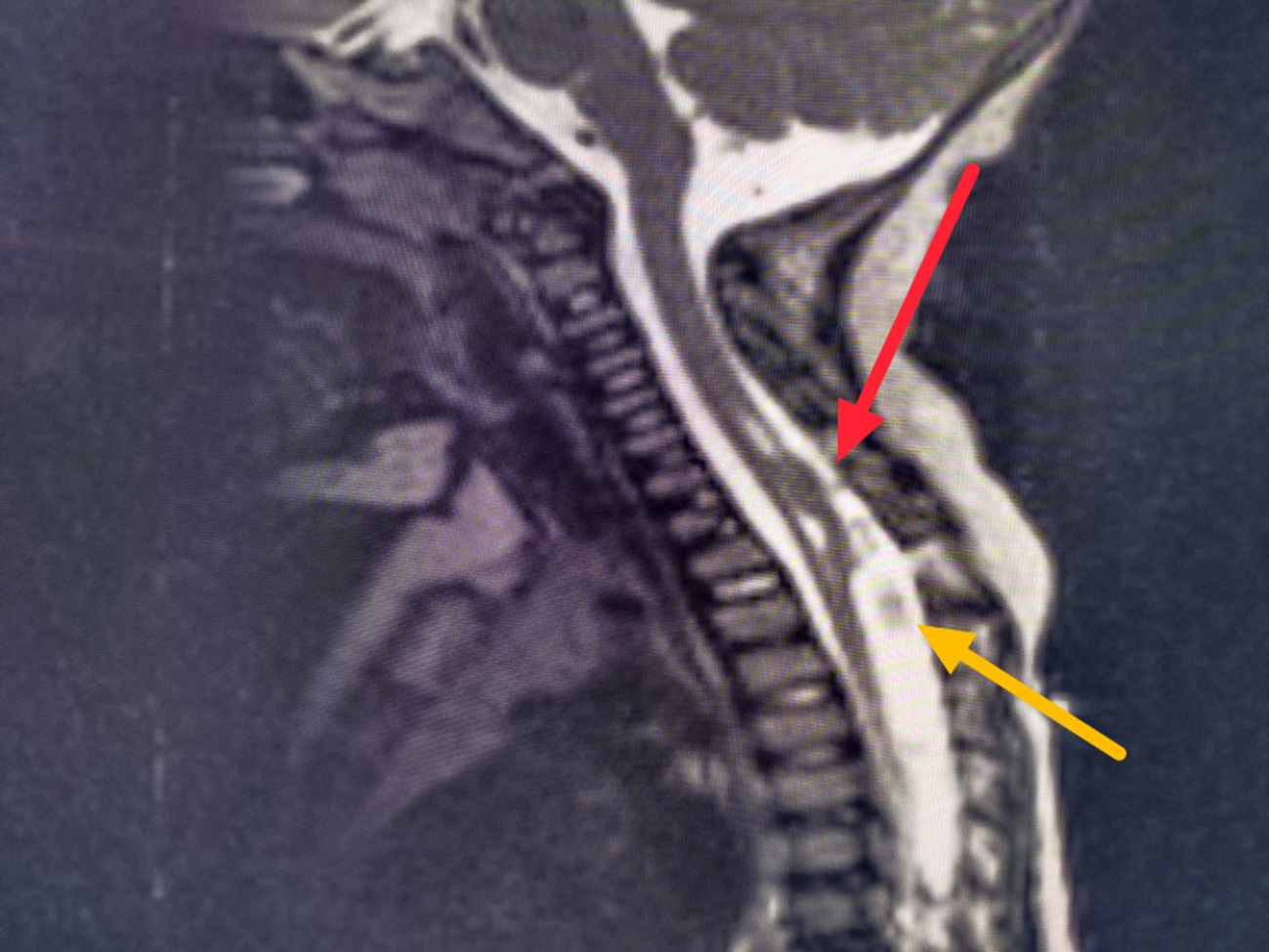
Fig. 3. Representative T2W MRI cut showing tethering at D3/D4 due to a band (red arrow) level with associated syrinx, yellow arrow points to protuberant arachnoid
The plan was to operate in two setting in view of the age and low weight of the child, the first stage, the patient underwent DV2 to DV5 laminoplasty and durotomy, per-op there was protuberant arachnoid membranes forming multiple arachnoid cysts which was dissected out and a single dorsal band arising from the dorsal aspect of the cord to the dura (Fig.4), which was carefully cut and after these dissections the cord settled down. Post-op the patient was managed in the paediatric ICU, there were no fresh neurological deficits, drain was removed on the third day and the patient was discharged on the 7th post-op day.
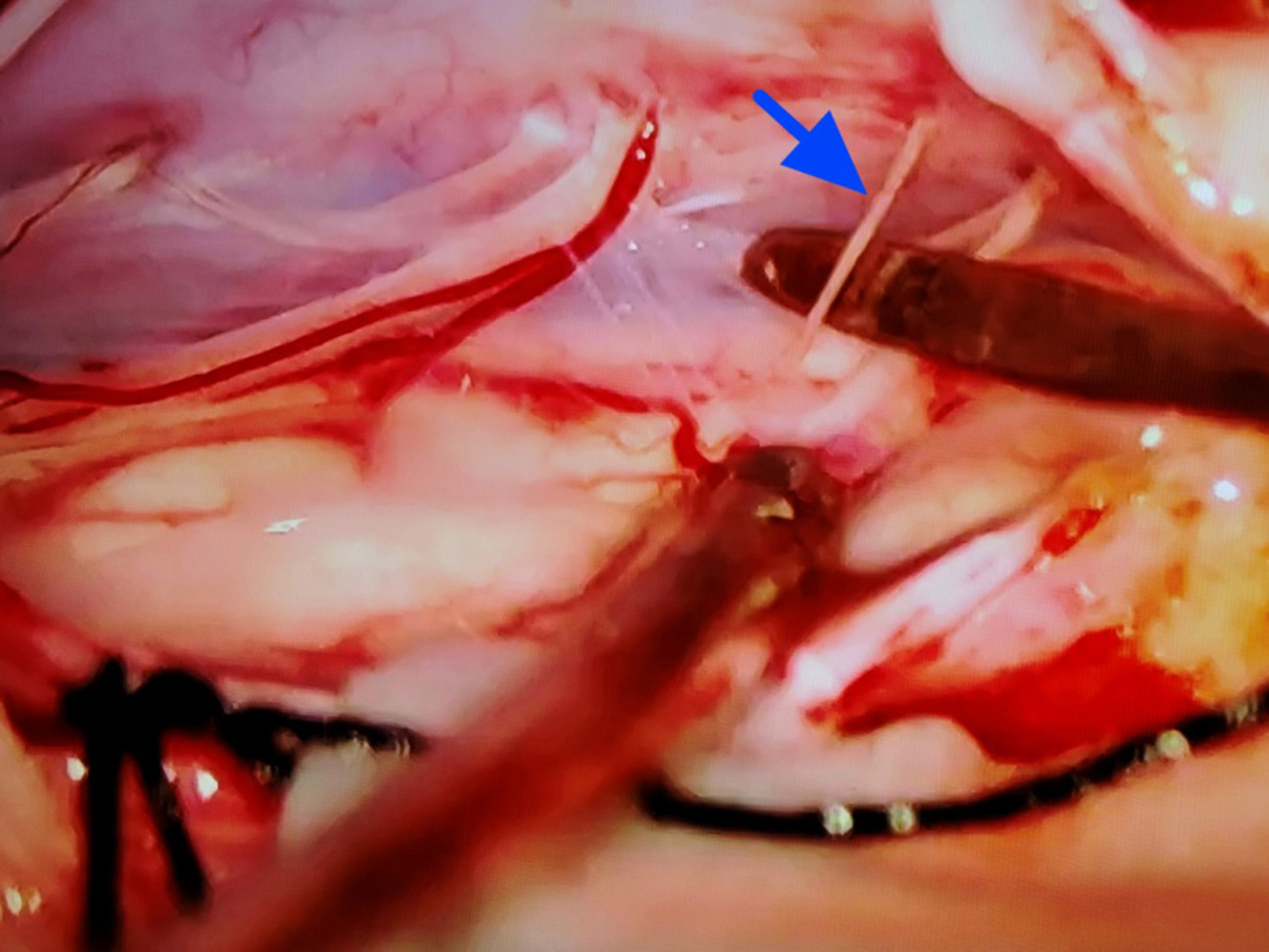
Fig. 4. Per-op photograph showing the dorsal band above the dissector on the right of the frame (blue arrow)
Review of literature
Meningocele manqué is basically tethering due to fibrous bands having atretic neural tissue. It is an incidental finding seen in spinal dysraphism [1, 2].
“Meningocele manque” was coined by James and Lassman in 1972. This was used to describe in patients with spina bifida occulta who had atretic meningoceles, and since there was no meningocele sac, this term was chosen. “Manque” which in French means ‘might have been but it is not’ [3].
Initially this term was used only to refer dorsal tethering bands found in cases of spina bifida occulta, but recently it’s also being used in dorsal tethering bands associated with meningocele. It is also seen associated with diastematomyelia and dermoid cysts. Literature on meningocele manqué is very limited [4].
Embryonic theory of meningocele manqué is not clearly defined; a possible hypothesis is the dysraphic defect in meningocele formation which atrophies and the remaining embryonic remnants of the atrophied meningocele form dysplastic nervous and fibrous tissue tethering the cord [5]. The exact cause of meningocele manqué is not known, the causes could be congenital malformation of the spinal cord, Vitamin B12 deficiency or could be an association with diastematomyelia. In meningocele manque, the herniated lesion can contain atretic neural tissue, meninges and CSF [6].
Symptomatology is usually neurological symptoms of tethered cord with cutaneous stigmata.
The differential diagnoses for meningocele manqué are meningocele and meningomyelocele. Meningocele manqué in isolation carries a good prognosis [7]. It is essential to detect it in the screening MRI and will have to be addressed before the formal surgery for other dysraphism, if not the retracting cord after de-tethering can get sheared/tugged at the site of meningocele manqué. A similar situation was found in our case; the child underwent successful release of the meningocele manqué at DV2/DV3 level and in second stage will undergo surgery for Lipomyelomeningocele.
Conclusion
Meningocele Manque is rare, it can present in isolation or associated with other spinal dysraphism. With other spinal dysraphism they can be either at the same or at another location, as was seen in our case. Before operating all cases of spinal dysraphism it is of paramount importance to MRI screen the entire neuraxis and study images thoroughly. In our case along with the dorso lumbar lipomyelomeningocele, there was a Meningocele manqué at DV3/DV4 level. It is essential that the meningocele manqué be addressed first; if not the returning/recoiling cord after de-tethering at the lower level can get tugged/sheared at the tethered meningocele manqué causing deficits.
Disclosure
Conflict of interest
None reported.
Informed consent
The patient's parents provided informed consent for the publication of data and images.
Funding
The author declares no financial support of any kind received for this study.
References